Plantar fasciitis, plantar heel pain, plantar fasciopathy – this condition has many names, a substantial negative impact on patients, and no single effective treatment. In this blog, we will explain our trial, The FIX-Heel Trial, which was recently published in BJSM. In this trial, we compared some of the most commonly used treatments for patients with plantar fasciopathy (1).
Why is this study important?
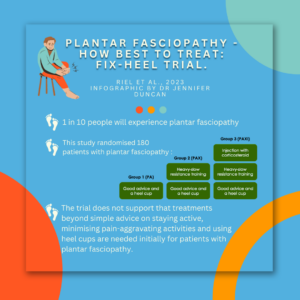
Across the lifespan, one in every ten of us will experience plantar fasciopathy, which makes it a very common musculoskeletal condition. Most patients will experience sharp pain under their heel when they first get out of bed in the morning or after sitting for a while. Even though it is a commonly held belief that this condition improves on its own, recent studies show that some patients still have pain for several years, even after treatment.
Several treatment options are available, but there is no evidence of any single treatment being substantially better than the other options. A corticosteroid injection may offer short-term pain relief, but there is no added benefit compared to a placebo after 6 to 8 weeks. In recent years, heavy-slow resistance training has emerged as a promising approach to treating plantar fasciopathy, drawing inspiration from its success in treating various other lower-limb tendinopathies. Resistance training is believed to be a potent stimulus for the healing of connective tissues. Heavy-slow resistance training for plantar fasciopathy initially displayed encouraging results compared to plantar fascia stretching. Nevertheless, it is important to note that the beneficial effects of this training regimen may not be immediately apparent to patients. This type of exercise typically requires some time to manifest and is mostly considered beneficial for long-term recovery from tendinopathies. Consequently, a potential strategy for improved treatment outcomes could involve combining both resistance training and a corticosteroid injection, offering patients both short-term and long-term relief from pain.
How did the study go about this?
We randomised 180 patients with plantar fasciopathy to either 1) Patient Advice and a heel cup (PA), 2) PA and heavy-slow resistance training (PAX), or 3) PAX and a single corticosteroid injection (PAXI) and followed them for one year (Figure 1). The exercise used was a heel raise exercise where patients stood with the forefoot on a step or a large book and placed a rolled-up towel underneath the toes. They were asked to perform the exercise for as many sets as possible every other day and continue to perform the exercise until they felt they had reached a self-evaluated acceptable symptom level and then for an additional four weeks. We used the change from baseline to the 12-week follow-up in the pain domain of the Foot Health Status Questionnaire as the primary outcome.

Figure 1: 3 groups in study
What did the study find?
We found no clinically relevant difference in the pain domain of the Foot Health Status Questionnaire between PA and PAXI after 12 weeks despite a statistically significant difference. There were no differences between either PA and PAX or PAXI and PAX. After one year, the difference between PA and PAXI was even smaller and less relevant.
What are the key take-home points?
The trial does not support that treatments beyond simple advice on staying active, minimising pain-aggravating activities and using heel cups are needed initially for patients with plantar fasciopathy. The results indicate that combining a corticosteroid injection with exercise is not superior to exercise or no exercise.
References:
- Riel H, Vicenzino B, Olesen JL, et al. Does a corticosteroid injection plus exercise or exercise alone add to the effect of patient advice and a heel cup for patients with plantar fasciopathy? A randomised clinical trial. British Journal of Sports Medicine 2023;57:1180-1186.
Author and affiliations
Henrik Riel, Bill Vicenzino, Michael Skovdal Rathleff
Henrik Riel, PhD, Center for General Practice at Aalborg University, Aalborg, Denmark
hriel@dcm.aau.dk