From prevention to rehabilitation; learning to safely return patients to exercise during covid-19
Despite comprehensive guidance on “return to sport” in elite athletes (1), there are currently limited recommendations to help clinicians return non-athlete populations to exercise post COVID-19. We discuss some of the challenges facing clinicians who are prescribing exercise to treat long term conditions (LTCs), or to rehabilitate patients during the current pandemic.
The impact of lockdown on Physical Activity
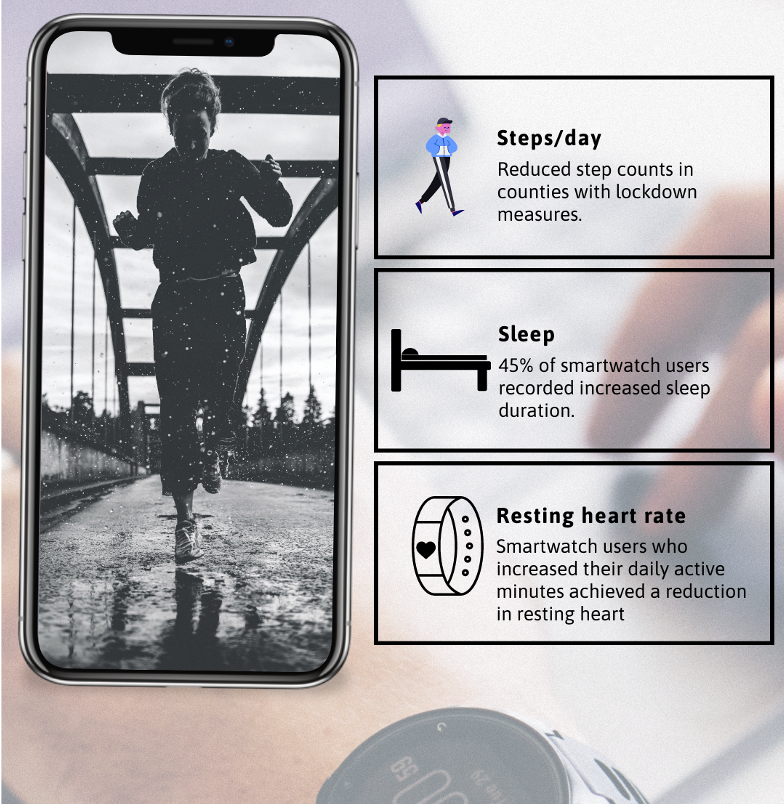
Government imposed lockdowns have drastically changed the health behaviours and PA levels of populations worldwide. Reduced time physically active, increased sleep duration, weight gain and reduced step counts have been recorded by smartwatch users across Europe and North America (2, 3, 4) (Figure 1). Concurrently, studies have shown that physical inactivity, obesity and non-communicable diseases are associated with worsening COVID-19 outcomes (5, 6). With the threat of a second wave or further lockdowns there is a risk that lockdown-associated behaviour changes may become habitual as we embrace a “new normal” way of life. For many the loss of exercise from daily commutes, the loss of face to face social interaction at work and organised social sports has restricted opportunities to lead healthy lifestyles; these changes may also significantly increase the risk of individuals developing preventable LTCs.
Figure 1: Trends in smartwatch users during lockdown (2, 3, 4)
Continuing to promote Physical activity during a pandemic
In order to reverse the trend of physical inactivity and promote the benefits of exercise on a population level, governments, healthcare systems and clinicians will need to think of innovative ways to promote the benefits of individual staying physically active. This may involve the use of health promotion materials, activity monitor technology, local policies to promote active commuting, and advice on healthy diets alongside exercise. Delivering, monitoring and safely prescribing exercise at scale during the pandemic is likely to be a significant challenge; as new data is revealing that covid-19 infection is associated with significant levels of disability and deconditioning post infection. Data from the Centre for Disease Control (CDC) reported that 35% of (outpatient) COVID-19 positive patients are not back to their usual state of health 2-3 weeks after infection (7). Further studies on hospitalised patients have reported “long covid” presentations, with 88% of patients reporting at least one persisting post covid symptom (mean follow up – 60 days) (8). These included exercises limiting fatigue, dyspnoea, joint pain, cough and chest pain.
Return to exercise protocols
Many of these post-COVID-19 symptoms are relative contra-indications to exercise and will impact the key physiological markers traditionally used by patients and clinicians to safely monitor exercise tolerance such as heart rate responses, ratings of perceived exertion, ratings of dyspnoea or the sing-talk test. The presence of “long covid” symptoms may also mask the presentation of more severe post COVID-19 cardiac or respiratory conditions; leading to some clinicians advising patients on absolute rest for prolonged periods.
If exercise clinicians are to deliver on the promise of tackling obesity and physical inactivity, they will need to consider designing new “return to exercise” guidelines for the non-athlete (general population). These guidelines will need to reflect the local resources (access to investigations and specialist referral pathways) available to primary care physicians who are managing the care of these patients increasingly via remote video or telephone consultations in the community. They will also need to take into account the age profile (increased average age), presence of pre-existing conditions, and functional needs of patients who may not have been exercising regularly or have pre-covid baseline investigations available to compare to.
As the NHS looks to provide tailored rehabilitation post covid-19, a key challenge will be to better understand the community rehabilitation needs and clinical course of recovery of patients in the post-acute phase of COVID infection (9). This will include validating new and existing measure of exercise intensity, so that patients can be safely guided from a period of rest post COVID to a gradual return to function & exercise.
Conclusion
The COVID-19 pandemic has once again revealed the underlying health impact of non-communicable diseases across the population. In order to reduce long term health inequalities and the immediate burden of COVID-19, exercise clinicians will need to design new rehabilitation programmes that incorporate validated “Return to Exercise” protocols for the general population.
Key Points
- Physical inactivity and obesity are associated with worsening COVID-19 severity and increased levels of disability post infection.
- “Long Covid” symptoms that are relative contraindication to exercise have been reported in hospitalised and non-hospitalised patients.
- New “return to exercise” protocols will be required to help guide the safe rehabilitation of patients in the general population (non-athletes).
Authors and Affiliations
Dr Aessa Mahmud Tumi
Dr Aessa Mahmud Tumi is a GP trainee on the St Mary’s vocational training scheme in central London. He has an interest in musculoskeletal, sports and exercise medicine. No conflicts of interest.
References
- Wilson MG, Hull JH, Rogers J, et al. Cardiorespiratory considerations for return-to-play in elite athletes after COVID-19 infection: a practical guide for sport and exercise medicine physicians. British Journal of Sports Medicine Published Online First: 02 September 2020. doi:10.1136/bjsports-2020-102710
- The Impact Of Coronavirus On Global Activity – Fitbit Blog [Internet]. Fitbit Blog. 2020 [cited 5 September 2020]. Available from: https://blog.fitbit.com/covid-19-global-activity/
- The Global Pandemic and Active Lifestyles – Garmin Blog [Internet]. Garmin Blog. 2020 [cited 5 September 2020]. Available from: https://www.garmin.com/en-GB/blog/the-global-pandemic-and-active-lifestyles/
- Heart Health Improves Even When Steps Decline – Fitbit Blog [Internet]. Fitbit Blog. 2020 [cited 5 September 2020]. Available from: https://blog.fitbit.com/covid-19-heart-health/
- Docherty Annemarie B, Harrison Ewen M, GreenChristopher A, Hardwick Hayley E, Pius Riinu, Norman Lisa et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study BMJ 2020; 369 :m1985
- Hamer M, Kivimäki M, Gale CR, Batty GD. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav Immun. 2020;87:184-187. doi:10.1016/j.bbi.2020.05.05
- Tenforde M, Kim S, Lindsell C, Billig Rose E, Shapiro N, Files D et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network — United States, March–June 2020. 2020. doi:10.15585/mmwr.mm6930e1
- Carfì A, Bernabei R, Landi F, for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020;324(6):603–605. doi:10.1001/jama.2020.12603
- NHS launches tool to aid long-term virus recovery [Internet]. BBC News. 2020 [cited 5 September 2020]. Available from: https://www.bbc.co.uk/news/health-53291925