An insight into the randomised, placebo-surgery controlled FIDELITY trial, as part of the BJSM’s new #KnowledgeTranslation blog series
Here we explain the latest 5-year results of our FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial, a placebo-surgery controlled trial that was launched in 2007. The full-text can be obtained here.
Introduction
The initial 1-year follow-up study, showing that arthroscopic partial meniscectomy (APM) provided no better symptom relief than placebo-surgery, was published in 2013 in the New England Journal of Medicine1. It may not be a huge exaggeration to state that the findings, practically eroding the evidence-base for the most common indication for the most common orthopedic procedure, were received with ‘mixed emotions’ in the orthopedic communities.
This brief video captures the chain of events that followed the publication of the FIDELITY 1-year data:
So, do we really need yet another study on this issue?
If no benefit for symptoms seems bad in its own right, things might be even murkier for the proponents of the APM procedure. Evidence from observational studies2 3 and some previous unblinded trials4-6 has lent support for concerns that in addition to being ineffective, APM might even cause harm in the form of accelerating the progression of knee osteoarthritis (OA). Given the legitimate concerns expressed regarding such inferences due to the nature of the previous data, we felt that our FIDELITY trial – given its novel placebo-surgery controlled design – was particularly fitted to overcome the concerns and address this pressing issue more definitely.
Additionally, given the existing strong voices that argue for the potential benefits of APM for ‘patients properly chosen for the procedure’, we felt that it would be a worthwhile effort to study the long-term effects, particularly as there exists some data to suggest that procedure may actually be associated with increased risk of progression of knee OA and subsequent need for “corrective” surgery.2 11
How was the FIDELITY trial carried out?
During a 5-year recruitment period, we screened more than 200 patients with knee symptoms consistent with degenerative medial meniscus tear and sent them all for an MRI scan. We ended up with 146 adults – who underwent either APM or placebo-surgery (Figure 1).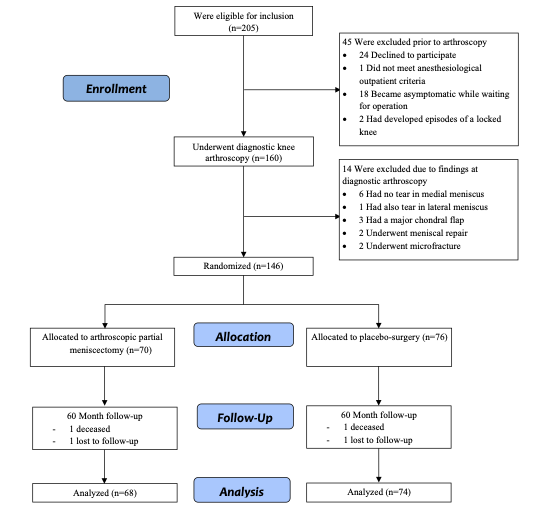
What did we discover?
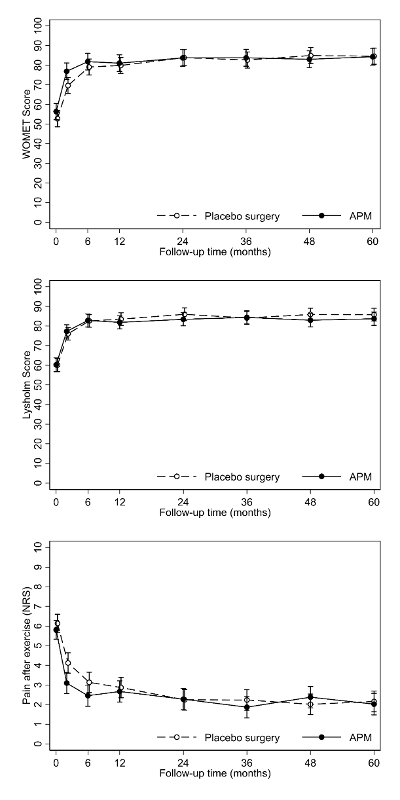
To make a potentially long story short, APM provided no more benefit for knee symptoms or function than placebo surgery in the three PROMs we used (Figure 2).
If no benefit on knee pain and function was something to be expected (based on the existing evidence, including the shorter-term findings of the FIDELITY trial), the most concerning finding of this study was that APM was associated with a slightly increased risk of developing radiographic knee OA at 5 years after surgery (Figure 3).
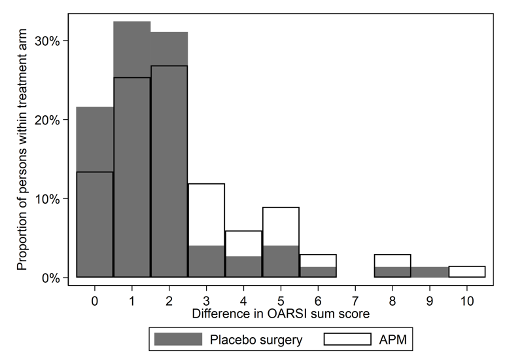
Figure 3: A histogram depicting the change in OARSI sum score from baseline to 5-year follow-up in the APM (blank bars) and Placebo-surgery (dark bars) groups. X-axis shows the difference between 5-year and baseline OARSI sum score, while the y-axis shows the percentage of participants with each change score, per treatment arm. The higher the bars are at the right end of the x-axis, the more participants with more advanced progression of OA (higher OARSI score).
Take-Home Messages:
Of note, only five years ago, the presence of ‘mechanical symptoms’ (sensations of knee locking or catching) was considered an ‘absolute’ indication for APM. We used our FIDELITY data14 15 to bust this widely-held contention. The 5-year data published now in the BJSM lend further support to the view that presence of ‘mechanical symptoms’ in a middle-aged and older patients are likely simply due to more advanced knee OA, and accordingly, should be considered a contraindication for APM. We hope that our results – suggesting an increased risk of development of knee OA – finally prompts this much-needed pendulum shift,. It truly is time to abandon ship and stop performing APM for middle-aged and older adults with knee pain.
Authors & affiliations:
Teppo L N Järvinen, professor1,2 (teppo.jarvinen@helsinki.fi)
Raine Sihvonen, consultant orthopedic surgeon1,3 (raine.sihvonen@fimnet.fi)
Martin Englund, professor4 (martin.englund@med.lu.se)
Simo Taimela, research director1,2 (simo.taimela@helsinki.fi)
1 Finnish Centre for Evidence-Based Orthopedics (FICEBO), University of Helsinki, Helsinki, Finland
2 Department of Orthopedics and Traumatology, Helsinki University Hospital, Töölö hospital, Helsinki, Finland
3 Pihlajalinna Koskiklinikka Hospital, Tampere, Finland
4 Faculty of Medicine, Department of Clinical Sciences Lund, Orthopedics, Clinical Epidemiology Unit, Lund University, Lund, Sweden
Competing Interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
References & Further Reading
- Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 2013;369(26):2515-24.
- Roemer FW, Kwoh CK, Hannon MJ, et al. Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol 2017;27(1):404-13.
- Rongen JJ, Rovers MM, van Tienen TG, et al. Increased risk for knee replacement surgery after arthroscopic surgery for degenerative meniscal tears: a multi-center longitudinal observational study using data from the osteoarthritis initiative. Osteoarthritis Cartilage 2017;25(1):23-29.
- Collins JE, Losina E, Marx RG, et al. Early MRI-based Changes in Patients with Meniscal Tear and Osteoarthritis. Arthritis Care Res (Hoboken) [Epub ahead of print] 2019 Apr 1
- Katz JN, Shrestha S, Losina E, et al. Five-Year Outcome of Operative and Nonoperative Management of Meniscal Tear in Persons Older Than Forty-Five Years. Arthritis Rheumatol 2020;72(2):273-81.
- Sonesson S, Kvist J, Yakob J, et al. Knee Arthroscopic Surgery in Middle-Aged Patients With Meniscal Symptoms: A 5-Year Follow-up of a Prospective, Randomized Study. Orthop J Sports Med 2020;8(1):2325967119893920.
- Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Ann Rheum Dis 2018;77(2):188-95.
- Hall MJ, Schwartzman A, Zhang J, et al. Ambulatory Surgery Data From Hospitals and Ambulatory Surgery Centers: United States, 2010. Natl Health Stat Report 2017(102):1-15.
- Abram SGF, Judge A, Beard DJ, et al. Temporal trends and regional variation in the rate of arthroscopic knee surgery in England: analysis of over 1.7 million procedures between 1997 and 2017. Has practice changed in response to new evidence? Br J Sports Med 2019;53(24):1533-38.
- Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ 2017;357:j1982.
- Winter AR, Collins JE, Katz JN. The likelihood of total knee arthroplasty following arthroscopic surgery for osteoarthritis: a systematic review. BMC Musculoskelet Disord 2017;18(1):408.
- Sihvonen R, Paavola M, Malmivaara A, et al. Finnish Degenerative Meniscal Lesion Study (FIDELITY): a protocol for a randomised, placebo surgery controlled trial on the efficacy of arthroscopic partial meniscectomy for patients with degenerative meniscus injury with a novel ‘RCT within-a-cohort’ study design. BMJ Open 2013;3(3)
- Sihvonen R, Kalske R, Englund M, et al. Statistical analysis plan for the 5-year and 10-year follow-up assessments of the FIDELITY trial. Trials 2020;21(1):76.
- Sihvonen R, Englund M, Turkiewicz A, et al. Mechanical Symptoms and Arthroscopic Partial Meniscectomy in Patients With Degenerative Meniscus Tear: A Secondary Analysis of a Randomized Trial. Ann Intern Med 2016;164(7):449-55.
- Sihvonen R, Englund M, Turkiewicz A, et al. Mechanical symptoms as an indication for knee arthroscopy in patients with degenerative meniscus tear: a prospective cohort study. Osteoarthritis and cartilage 2016;24(8):1367-75.