Building on last week’s podcast with Dr Mary O’Keeffe
On last week’s episode, we were joined by Dr Mary O’Keeffe to discuss how clinicians can better manage patients with low back pain. Mary is a physiotherapist and a Marie Skłodowska-Curie Postdoctoral Fellow. Mary was awarded her PhD in 2017, in which she examined multidimensional rehabilitation for the individual with chronic back pain. Mary’s research now focuses on changing clinicians’ behaviour, improving diagnostic labels of low back pain, and communicating healthcare messages in the media. In this 20-min podcast, Mary explores clinicians’ common misconceptions about low back pain and how we can better address psychosocial aspects of care. A really interesting take on such a prevalent condition with plenty of useful takeaways to add to your clinical arsenal!
What do we think are some of the biggest lessons from this podcast?
We know that Lower Back Pain (LBP) is a common cause of disability globally. Indeed, we know that many of those who suffer LBP suffer ‘relapsing-remitting’ courses where symptoms get worse, then can relieve for periods, before returning once again. Dr O’Keefe makes a strong case that a substantial proportion of people have persistent symptoms and generally speaking, we aren’t good at evaluating why the symptoms appear in the first place and which treatments best suit an individual’s needs.
- Framing the condition in an over medicalised way can create the illusion of easy fixes for a complex pathology, with many possible causes.
- Clinicians should be encouraged to feel confident in moving away from using tissue-based diagnosis to inform treatment for LBP. Imaging can sometimes do more harm than good. Red flag conditions, if suspected, such as Cauda Equina Syndrome, or fractures should be imaged and managed immediately, however, imaging can reveal incidental findings such as degenerative changes, or disc protrusions that could legitimise unnecessary medical intervention.
- We need to challenge the myth that back pain is caused by tissue damage and that exercise is dangerous to those suffering from LBP.
- Active listening to the patient’s story can help legitimise their symptoms. Over time this will help develop more trust between clinician and patient.
- Treatment needs to be individualised and focused on activity modification and empowering the patient to self-manage in the first instance. Clinicians should be creative in exploring ways to cut activities that the patient finds disempowering and encourage behaviours they enjoy.
This links well to the now classic infographic and editorial produced by Lewis, O’Sullivan and YLM Sport Science.
https://bjsm.bmj.com/content/52/24/1543

Want more resources on empowering patients to take control of their back pain?
Within the BJSM community we are lucky have to have access to some world class research on relevant collections on LBP management – enjoy!
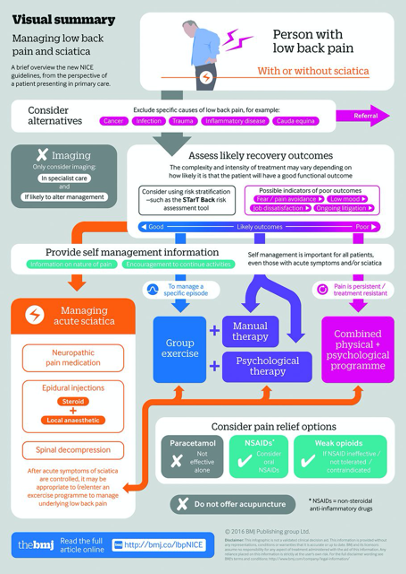
NICE low back pain guidelines: opportunities and obstacles to change practice
https://bjsm.bmj.com/content/51/22/1632
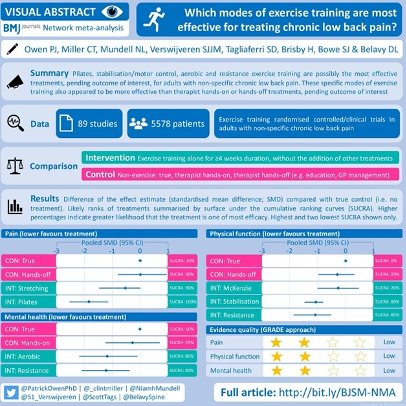
Infographic. What kinds of exercise are best for chronic low back pain?
https://bjsm.bmj.com/content/early/2020/06/15/bjsports-2020-102024
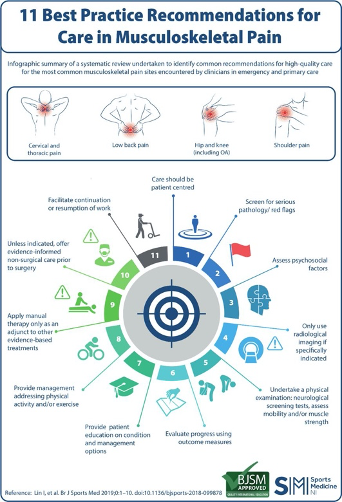
Infographic. 11 best practice recommendations for care in musculoskeletal pain
https://bjsm.bmj.com/content/53/19/1250
Infographic. Roadmap to managing a person with musculoskeletal pain irrespective of body region
https://bjsm.bmj.com/content/54/9/554

—
Author and Affiliations:
Blog by Jonny Elliott, Junior Doctor based in Belfast, Northern Ireland Representative Undergraduate Sports & Exercise Medicine Society (USEMS).