By Dr Nicky Keay @nickyKfitness
“We need to treat individual women, not statistics” was the concluding sentence of an insightful BMJ Editorial 2019 [1]
However, as Caroline Criado Perez points out in her recent, science prizing-winning book, ‘Invisible Women’, in many instances there are no scientific or medical statistics on women [2].
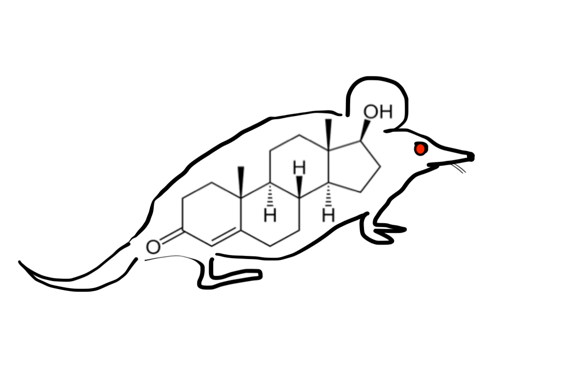
The efficacy of drugs is predominately initially tested in vivo on male cells. So at inception, potentially many medications, which might have been effective in females, are discarded at the earliest stage of research, because no effects are observed in male cells. The trend of the default male organism in research follows through into animal experimentation on male mice. Although animal models may not be entirely predictive of effects in humans, certainly the effects in female humans will be even less certain. Does it matter that research is conducted predominately on male tissue, male organisms and men? Thalidomide is a drug that had devastating teratogenic effects when taken by women. Indeed, a wide range of potential sex differences in the effects and metabolism of drugs has been reported. Furthermore, the action of drugs-including adverse effects-can vary according the phases of the menstrual cycle, due to variations in circulating sex steroids. For example, certain drugs are likely to cause arrhythmia in the follicular phase of the menstrual cycle [3]. The effect of many drugs in females is not well understood, as research had not included females, let alone women in different phases of the menstrual cycle.
Why is research focused on males?
Some researchers argue that the menstrual cycle in females is “too complicated” or including women in a study at difference phases of the menstrual cycle “will interfere with results”. Menstrual cycles have been around since women evolved, so this is not a phenomenon that is going to go away anytime soon. Therefore, welcoming the complexity of the intricate choreography of hormones during the menstrual cycle and during the lifetime of a woman, is a more constructive approach. Certainly a more acceptable scientific approach elucidates the similarities and differences between men, rather than excluding the female half of the population and assuming no differences in physiology and metabolism exist. Furthermore there are differences between individual women. Individual women will be impacted by fluctuations of hormones during the menstrual cycle in different ways, depending on varying tissue sensitivities to steroids among individuals.
This concept is especially important in sports science where the vast majority of studies are conducted in males. As I outlined in my presentation recently at Barça Innovation Hub, before discussing the periodisation of external factors (training load, nutrition, recovery), researched in males, it is vital to take into account internal bio-chronometers[4]. For example, circadian misalignment leads to suboptimal health and performance[5]. For female athletes, the most important cyclical variation is the menstrual cycle. Furthermore, periodic changes in hormones have individual effects. Only when these are recognised can external factors be integrated with internal periodicity. In other words, taking account of individual internal variations makes it possible to provide personalised advice. Tracking menstrual cycles provides an important training metric as menstrual cycles are a barometer of healthy hormones [6]. As it becomes easier to track personal health and performance data on a daily basis, both researchers and individual women can gain a better understanding of how female physiology varies over the menstrual cycle. Optimising health and performance for the individual female athlete makes for a stronger team.
What about in the clinical medical setting?
I recently attended an excellent update on acute medicine for medical doctors. An eminent cardiologist presented a series of case studies, including a woman who started experiencing symptoms in the morning, which both she and doctors thought were due to indigestion. Eventually when this “indigestion” had not settled by later afternoon, she attended the Accident and Emergency (A&E). She had suffered an extensive myocardial infarction (heart attack). The cardiologist explained that even though she went to a hospital with an on-site primary percutaneous coronary intervention facility, unfortunately due to the long delay in presenting to hospital, the heart muscle had died. The medical doctor had missed the opportunity to take her into the catheterisation laboratory to restore blood flow and function to the cardiac muscle. He outlined how this delay in diagnosis would have a big impact on her future quality of life and life span. Unfortunately this is not an isolated case. Women are far more likely to be misdiagnosed as not having acute coronary syndrome, when in fact they are indeed suffering a “heart attack”. Why is this? The “typical” presentation of myocardial infarction of central crushing chest pain with radiation to left neck and arm, disseminated to the public and medical students, is in fact only typical for men. Women present with “atypical” symptoms- which are atypical for men [7].
Even where female specific statistics do exist, the emphasis should be on considering the individual woman in clinical context. The recent BMJ editorial on HRT emphasised providing women with high quality, unbiased information on which women can weigh up their personal risk/benefit outcomes from HRT. As every woman can experience changes in hormones differently, including those occurring at the menopause; the emphasis should be on an individual woman’s quality of life, rather than epidemiological statistics [1].
There are important differences between mice, men and women.
***
Dr. Nicky Keay (@nickyKfitness) BA, MA (Cantab), MB, BChir, MRCP. Honorary Fellow Dept Sport and Exercise Sciences, Durham University.
This blog was republished from here: https://nickykeayfitness.com/blog/
References
[1] Rymer J, Brian, K, Regan L. HRT and breast cancer risk. BMJ Editorial 2019. dx.doi. org/10.1136/bmj.l5928
[2] Caroline Criado Perez. Royal Society Book Prize. Invisible Women. Publisher Chatto & Windus 2019
[3] Soldin O, Chung S, Mattison D. Sex Differences in Drug Disposition. Journal of Biomedicine and Biotechnology 2011, Article ID 187103 doi:10.1155/2011/187103
[4] N. Keay “Dietary periodisation for female football players” Barca Innovation Hub conference, Camp Nou, Barcelona, 9 October 2019
[5] N.Keay, Internal Biological Clocks and Sport Performance BJSM 2017
[6] N.Keay, What’s so good about Menstrual Cycles? BJSM 2019
[7] Khamis R, Ammari T, Mikhail G. Gender differences in coronary heart disease. Education in Heart. Acute coronary syndromes. BMJ Heart http://dx.doi.org/10.1136/heartjnl-2014-306463