The excellent RESTORE trial has just been published in JAMA1 – it was my most eagerly awaited publication of 2021. This was a Randomised Control Trial (RCT) of Platelet Rich Plasma (PRP) injections vs placebo saline for mild-moderate knee osteoarthritis (OA) with a protocol pre-published, high enrolment, good blinding and MRI pre- and post- assessment. It is definitely the best quality RCT published on the topic to date, and for this the authorship team, led by Kim Bennell, deserve enormous kudos1. It is worthy of a JAMA publication. And the headline finding is that PRP injections did not provide significant benefits over placebo injections. The study overall is worthy of further analysis however, and personally I don’t think that it “nails the coffin shut” on PRP injections for knee OA, as some detractors claimed on Twitter. It will be a hard coffin to nail shut when there are multiple systematic reviews and meta-analyses (pre-RESTORE) showing benefit.2-6

Key findings of RESTORE
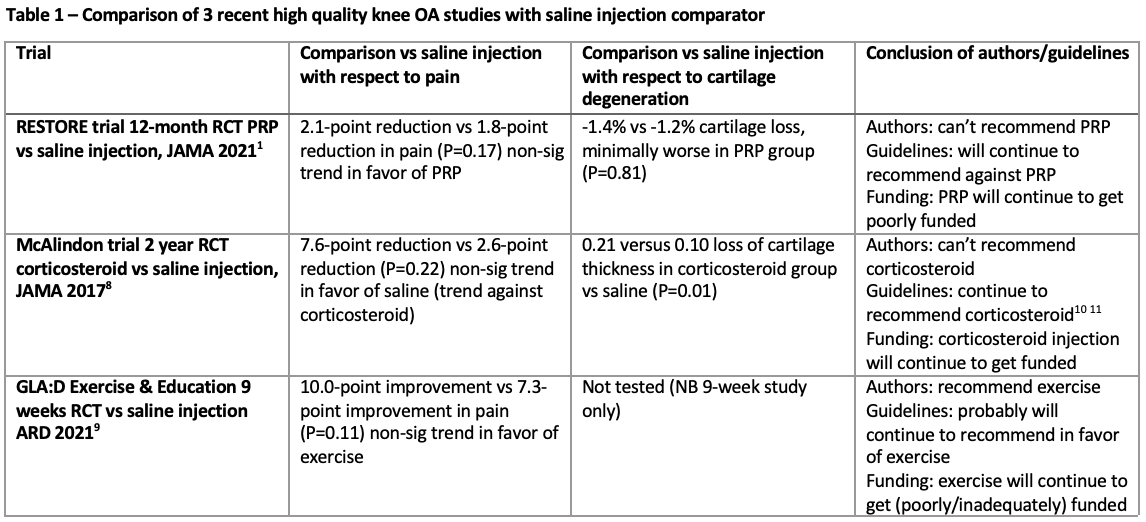
The most definitive finding from the RESTORE trial was that there were very similar results between PRP and saline injections in terms of further cartilage degeneration on MRI scan at 12 months, and splitting hairs if anything the results minimally favoured saline, although there was a p value of .81 for the primary outcome (81% likelihood that chance explains this tiny difference). I would agree with the authors that this study rules out the studied PRP regime as being a biological cure (disease modifying) for knee OA (i.e. PRP doesn’t protect or restore knee cartilage), although a previous (lower quality) study did find some imaging improvements on MRI7. Clutching at a positive, PRP doesn’t appear to degenerate knee cartilage any more than normal saline does. This finding does not apply to the “Gold standard” injection for knee OA (corticosteroid) which most definitely does cause additional cartilage degradation beyond normal saline8. Just as RESTORE is now the best quality study of PRP injections for knee OA, the McAlindon study of 2017 in the same journal is the best quality study of corticosteroid injections for knee OA. It conclusively showed cartilage degeneration at two years with corticosteroid (RESTORE only followed up for one year with PRP) 8.
The more subtle finding of RESTORE was that there was a trend towards improved clinical outcomes in the PRP group. With respect to the primary outcome – pain at 12 months – this did not reach statistical significance. The PRP group had slightly better results than saline, but there was a p value of 0.17 for the primary outcome, meaning a 17% chance that this difference was due to chance, but therefore an 83% chance that PRP did show slightly better pain results in this trial. For the secondary outcome of Global improvement, this favoured PRP significantly over saline at two months with a p value of 0.02 with a strong trend towards better Global improvement at 12 months (P=0.09).
Author interpretation of RESTORE
This is where the author interpretation is fascinating. Many author groups tend towards Type I errors, with some data mining through secondary outcomes until they find a significant result, in the hope that a headline positive finding will be more likely to get the paper more prominence. The RESTORE authors had some significant findings hiding in plain sight in their secondary outcomes, with a matching trend in one of their primary outcomes that was more likely to be a true difference in the groups than due to chance. Not only did they pass on the opportunity to claim that there possibly was a potential benefit for PRP in terms of clinical outcomes, they went in the full other direction and stated that there definitely was no benefit over placebo. Interestingly they made no comment on whether they thought the benefits found in the Secondary Outcomes were due to chance (which seems less likely) or inadequate blinding in the RESTORE study (for which they criticised the other previous studies showing benefits of PRP vs saline), given that they have discounted that this finding could possibly be due to true (albeit small) therapeutic effect. This is their study and their right, but it can be noted that it puts them in opposite camp to most other authors in that they risk a Type II error of ignoring a potential real difference between the groups. As a fascinating comparison, a similar “hot off the presses” article comparing “Exercise and Education” to normal saline injections for knee OA9 found similar results to RESTORE (a non-significant trend towards the index treatment over saline). The author group is arguing to strongly advocate for the index treatment based on the trial results, the opposite conclusion to the RESTORE authors (Table 1).
Data is data and I have 100% trust in the RESTORE author group to have faithfully reported their results, but the interpretation of results is part of a culture war that is set to continue which I will explain in a follow-up blog post. The next phase of the culture war will be updated systematic reviews and meta-analyses. If you combine the RESTORE results (a slight trend towards pain benefit of PRP for knee OA) with some or all of the previously published RCTs (almost all of which showed more substantial benefits), you are likely to end up with a further finding of meta-analysis benefit for PRP in knee OA. Alternatively, you could perform a systematic review and exclude the more than 20 other previously published studies based on inferior quality to RESTORE, and conclude that there is only one decent study on PRP in knee OA and it showed no overall benefit. Perhaps a fair (balanced) systematic review finding would be that the more you improve blinding, the less that there appears to be a therapeutic effect comparing PRP to saline, but even the gold standard trial to date has not managed to completely eliminate it (pain benefit of PRP vs saline).
Conclusions
My conclusions (opinions) are:
- That RESTORE strongly finds there is no disease-modifying (cartilage preserving) benefit of their PRP regime in knee OA
- That between RESTORE and other trials there is a small but non-zero benefit of PRP on pain over 12 months vs saline
- ….with no complications or known downsides but with moderate costs of treatment
- I’m less concerned than some critics that RESTORE may have chosen the “wrong” PRP protocol, and that others may have greater effect. I don’t think it is fair to argue this after you’ve seen results that were disappointing.
- Post-RESTORE it is hard to justify PRP as a universal treatment for knee OA or even a highly cost-effective one, but nor should it be completely discarded
- I am surprised at how keen mainstream medicine (i.e. guidelines) discount any possibility of PRP being used for knee OA, when the same guidelines still support corticosteroid injection10 11 (which clearly has worse outcomes to PRP and exercise). More on this in a follow-up Blog
Author and Affiliations:
John Orchard @DrJohnOrchard AM MD PhD FACSEP FFSEM (UK) FACSM
References
- Bennell KL, Paterson KL, Metcalf BR, et al. Effect of Intra-articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis: The RESTORE Randomized Clinical Trial. Jama 2021;326(20):2021-30.
- Nie LY, Zhao K, Ruan J, et al. Effectiveness of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Clinical Trials. Orthopaedic journal of sports medicine 2021;9(3):2325967120973284.
- Laudy A, Bakker E, Rekers M, et al. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med 2015;49(10):657-72.
- Hohmann E, Tetsworth K, Glatt V. Is platelet-rich plasma effective for the treatment of knee osteoarthritis? A systematic review and meta-analysis of level 1 and 2 randomized controlled trials. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie 2020;30(6):955-67.
- Dai WL, Zhou AG, Zhang H, et al. Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Trials. Arthroscopy 2017;33(3):659-70.
- Hong M, Cheng C, Sun X, et al. Efficacy and Safety of Intra-Articular Platelet-Rich Plasma in Osteoarthritis Knee: A Systematic Review and Meta-Analysis. BioMed research international 2021;2021:2191926.
- Lisi C, Perotti C, Scudeller L, et al. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil 2017:269215517724193.
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. Jama 2017;317(19):1967-75.
- Bandak E, Christensen R, Overgaard A, et al. Exercise and education versus saline injections for knee osteoarthritis: a randomised controlled equivalence trial. Annals of the rheumatic diseases 2021.
- Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis & rheumatology (Hoboken, NJ) 2020;72(2):220-33.
- Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019;27(11):1578-89.