The SARS-CoV-2 pandemic has provided a constant challenge to sport with varying protocols and regulations across the globe. In October 2020, we published a graduated return to play protocol 1 to aid colleagues and athletes resume safe exercising and training ahead of return to competition. With the imminent Tokyo Summer Olympic and Paralympic Games, it was considered that we could convey our experience of managing recently infected elite athletes during the early stages of the pandemic and showcase the evolution of best-practice for the safe return of athletes to sport.
As the pandemic progressed, additional research was published describing the typical presentation of SARS-CoV-2 infection, the impact on athletes and more detailed outcomes from cardiac and respiratory assessment2.
In elite sport, one of the biggest challenges is keeping care patient-centred yet advising coaching colleagues on relevant medical information, within the boundaries of patient confidentiality. The creation of an easy-to-follow graduated return to play (GRTP) plan helps inform all involved in the care and support of an athlete. It provides easily accessible guidance on what would be deemed normal to expect in the resumption of physical activity and training reflecting case management experience and the relevant published research. It has been our experience that sharing the GRTP with athletes and non-clinical colleagues has created greater understanding on how to manage novel respiratory infections in elite sport settings.
We continue to learn as the pandemic ebbs and flows across the globe. Published evidence from our elite athlete cohort 2 suggests that COVID-positive athletes who are either asymptomatic or only experience ‘above neck’ symptoms (e.g. cough, loss of taste or smell) tend to recover more quickly and thus may be able to safely resume full training quicker than athletes who experience ‘below neck’ or more systemic symptoms (including, but not limited to: fever, shortness of breath, chest pains or palpitations). In addition, other studies have shown that cardiac complications arising from SARS CoV-2 infection are usually associated with the presence of symptoms that signpost or localise to the lower chest during the acute illness and with ongoing lower chest symptoms and abnormal cardiovascular findings (e.g. increased HR) on return to exercise 3. We were keen, with both the original GRTP and these updated protocols, to highlight symptoms of possible concern that should be brought to the attention of the supervising clinician (figure 2).
Before commencing this updated GRTP protocol (figure 1), all athletes must be able to complete all activities of daily living without excessive fatigue and/or breathlessness and be able to walk on the flat without getting breathless. This guidance is not appropriate for athletes who have been hospitalised or required acute emergency care; in this scenario clinician led case-by case GRTP planning is recommended.
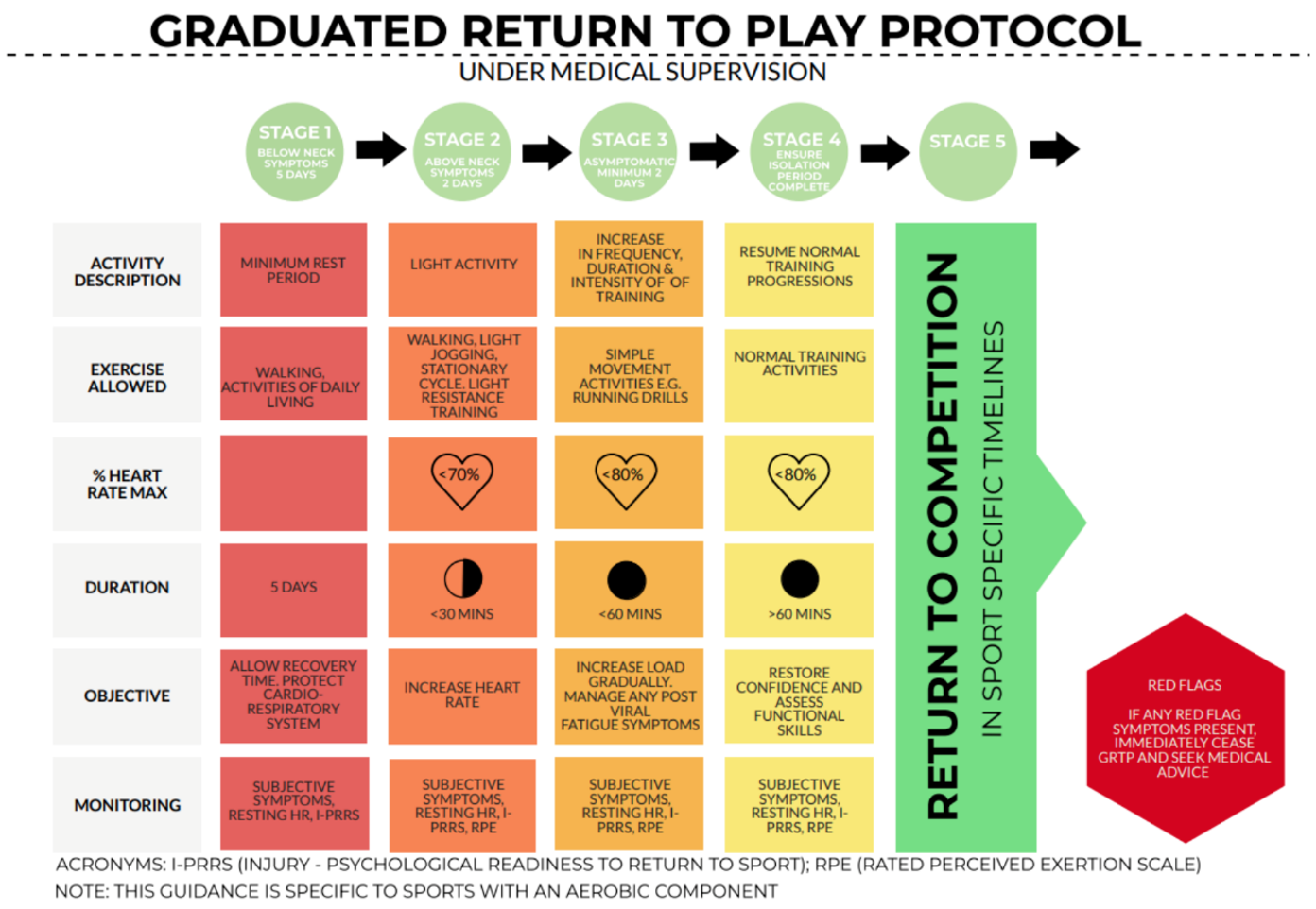
For athletes who experience any ‘below neck’ symptoms, their GRTP protocol starts at STAGE 1 with a minimum of 10 days to completion. It involves complete rest for at least 5 days to optimise the initial recovery and protect the cardio-respiratory system. After this initial 5 days of rest, if symptoms are improving satisfactorily, and the supervising clinician approves, the GRTP can continue into STAGE 2 (a minimum of 48hrs of light activity), then progresses through STAGE 3 over a minimum of 48hrs. As such, STAGE 4 (normal training resumption) could, in theory, be achieved as soon as day 10, and then STAGE 5 (return to competition) thereafter, at the discretion of the supervising clinician and wider support team.
For athletes who have mild above neck symptoms only it is recommended that the GRTP has a minimum of 5 days to completion. Their GRTP protocol starts at STAGE 2 (i.e. an athlete can continue to undertake light activity). After 48hrs, this progresses through STAGE 3 over a minimum of another 48hrs. As such, STAGE 4 (normal training resumption) could, in theory, be achieved as soon as day 5, and then STAGE 5 (return to competition) thereafter. The mandatory self-isolation period should be fully adhered to (e.g. even if STAGE 4 commences before the end of the self-isolation), and all of these progressions are at the discretion of the supervising clinician and wider support team.
Athletes that test positive yet are asymptomatic should start at STAGE 3 and be closely monitored throughout the GRTP for the development of signs (HR, HRV, RPE etc) and symptoms that may be associated with Covid-19. If they develop symptoms, they should return to STAGE 1 or STAGE 2 depending on clinical presentation.
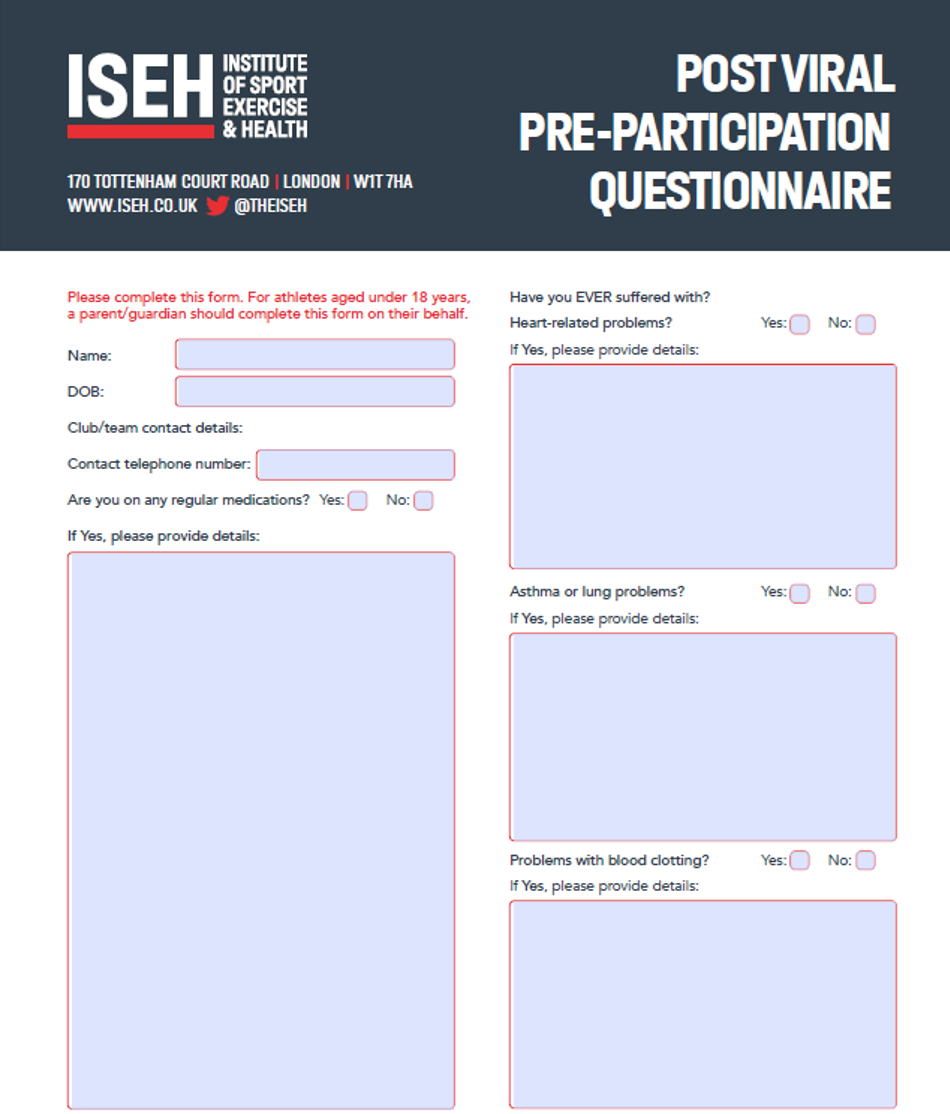
In all cases, if any of the ‘red flag’ symptoms manifest (figure 2) or if the athlete or anyone else supporting them has any concerns, the supervising clinician should be consulted immediately, and the GRTP should be ceased. A questionnaire can be used to formally document the absence of any warning features (see figure 3 as an example). Some people take over 3 weeks to recover and return to full training, and some mild symptoms may also persist (e.g. mild breathlessness, fatigue, reduced or altered smell / taste), which may extend the return to training process.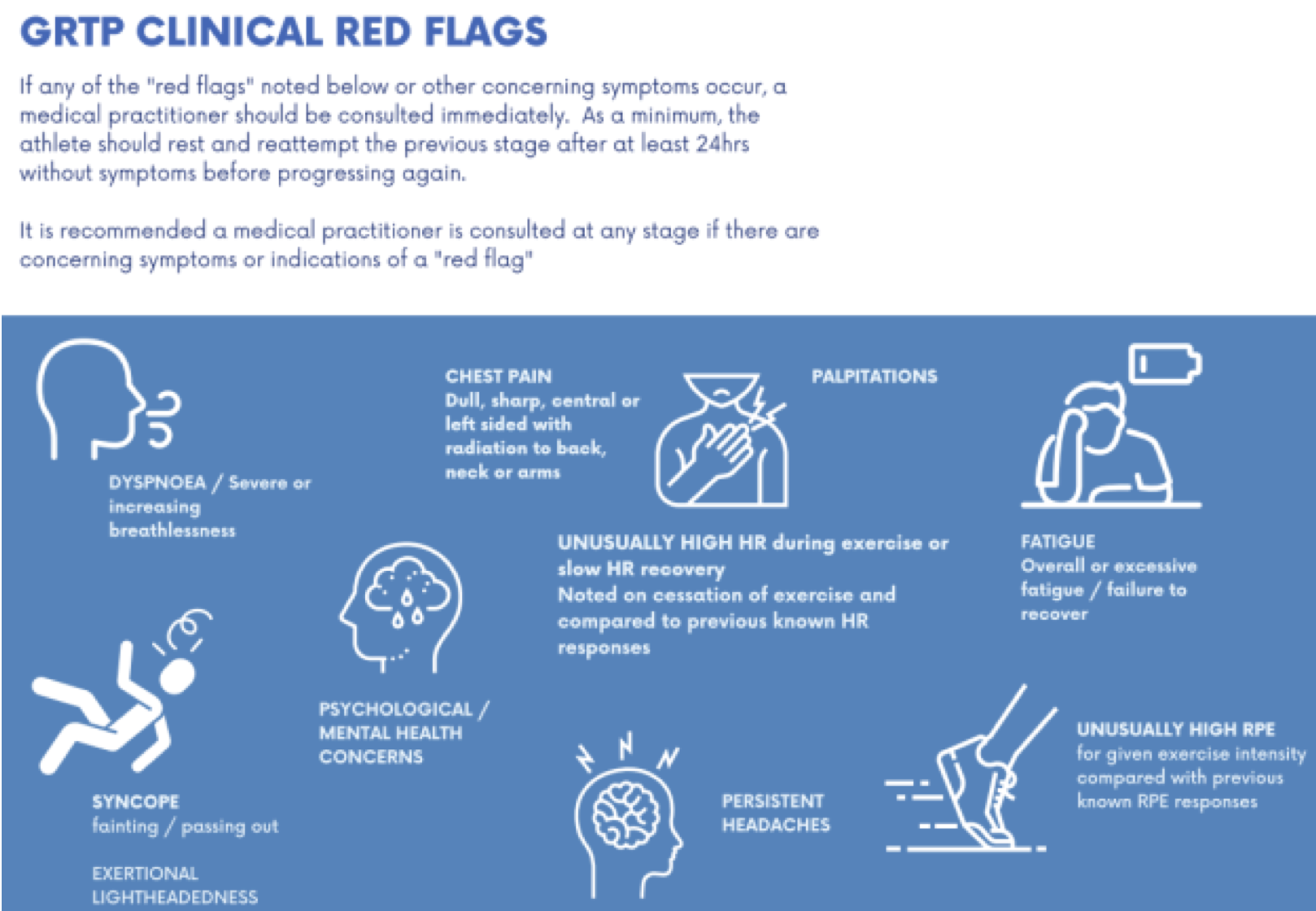
Conclusion
We have learned much and continue to learn from the SARS CoV-2 pandemic over the past 24 months. Thankfully, the majority of athletes now infected with SARS-CoV-2 do appear to suffer with a short-lived illness and make a rapid return to competitive sport. For SEM clinicians, recognising red flag or warning clinical features is vital to help guide return to training and competition using a safe framework; this is familiar to sports medicine practitioners in areas such as concussion. Our COVID GRTP framework has been adapted with knowledge of how SARS-CoV-2 impacts athletes and allows athletes to feel more confident in their resumption of training and sport.
References
- Elliott N, Martin R, Heron N, et al
Infographic. Graduated return to play guidance following COVID-19 infection. British Journal of Sports Medicine 2020;54:1174-1175.
- Hull JH, Wootten M, Moghal M, et al
Clinical patterns, recovery time and prolonged impact of COVID-19 illness in international athletes: the UK experience. British Journal of Sports Medicine 2022;56:4-11.
- Petek BJ, Moulson N, Baggish AL, et al
Prevalence and clinical implications of persistent or exertional cardiopulmonary symptoms following SARS-CoV-2 infection in 3597 collegiate athletes: a study from the Outcomes Registry for Cardiac Conditions in Athletes (ORCCA) British Journal of Sports Medicine Published Online First: 01 November 2021. doi: 10.1136/bjsports-2021-104644
Authors and Affiliations:
N Elliott1,2, A Biswas3, N Heron4,5, C Ranson6, J Hull7 , R Martin8, J Elliott9,10
- Sportscotland Institute of Sport, Stirling, UK
- Edinburgh Sports Medicine Research Group, Edinburgh, UK
- English Institute of Sport, Bisham Abbey, UK
- Sport Institute of Northern Ireland, Newtonabbey, UK
- Queens University, Belfast, UK
- English Institute of Sport, Bisham Abbey, UK
- Institute of Sport, Exercise and Health (ISEH), UCL, London, UK.
- Welsh Institute of Sport, Cardiff, UK
- Royal Victoria Hospital, Belfast, UK
- University of Bath, Bath, UK
Acknowledgements
We wish to acknowledge input received from colleagues from the Home Countries Institutes of Sport for the reviews and application of the guidelines. We also wish to recognise the Institute of Sport, Exercise and Health for use of their pre-participation questionnaire (figure 3) which can be found at https://www.iseh.co.uk/data/files/ISEH%20Post-viral%20questionnaire%202022.pdf