Key words: #MSKplaybook #Mindthesofttissuegap #frozenshoulder #MSKultrasound #SEM #Hydroditension
Introduction
Frozen shoulder (adhesive capsulitis) is a common condition within community musculoskeletal (MSK) interface services, which presents insidiously and significantly impacts patients’ quality of life and function.
In this blog, we discuss how a community-based pathway can permit early diagnosis through prompt referral to rehabilitation, alongside access to injection treatment and MSK ultrasound when there is diagnostic uncertainty. Close links with the shoulder orthopaedics team can also facilitate early escalation of patients with significant cuff tear or post-trauma.

Figure 1: The MSK playbook: frozen shoulder
Bringing a one stop shop model to the diagnosis of frozen shoulder
Frozen shoulder is associated with significant disability during the acute and post-acute phases. Patients can often present to various primary care clinicians – general practitioners, first contact practitioners, or practice-based physiotherapists, depending on local staffing and resources. This is a challenge for the early diagnosis and management of frozen shoulder, as not all primary care services have the capacity to offer regular reviews and continuous rehabilitation alongside potential injection therapies.
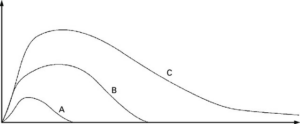
Figure 2: Natural history of frozen shoulder(1)
A – Short episode of frozen shoulder with full resolution of symptoms
B – Frozen shoulder with resolution of symptoms
C – Prolonged episode of frozen shoulder with chronic long-term deficit
Frozen shoulder has a natural timeline for improvement; however, early diagnoses can assist patients to navigate treatment options. In short lived episodes or mild symptoms, this may mean a full resolution of symptoms with rehabilitation +/- injection therapy. In cases where the symptoms are more significant, prolonged or chronic, clear referral links for hydrodistension, and early treatment is key for accelerated recovery. Suprascapular nerve blocks can also be considered if there is appropriate expertise available.

Figure 3: Summary of the initial phase of the community based MSK pathway for frozen shoulder
A focussed clinical history, examination, and X-ray (two views) can be used to rule out osteoarthritis; in most cases, this will confirm the diagnosis. However, if there is a suspicion of a significant rotator cuff tear (trauma) or tendinopathy, MSK ultrasound can help to rule in or rule out this diagnosis.
Background
- Frozen shoulder is classified as either primary or secondary:
- Primary: spontaneous onset with no known cause or trauma.
- Secondary: associated with trauma, prolonged immobility, surgery or other pathology, such as sub-acromial pain (2).
- It is characterised by fibroproliferative tissue fibrosis (formation of scar tissue, adhesions and capsular thickening) (2,3).
- Frozen shoulder has an incidence of 3-5% in the general population (4), which may be as high as 20% in individuals with diabetes (5).
- Frozen shoulder often has a varying presentation, with evolution of symptoms over time.
- Typically, it is a self-limiting disease that resolves within 1-3 years, although 20-50% of patients may develop chronic symptoms (3).
- Up to 6% of patients report severe symptoms >7 years after symptoms begin (6).
- In up to 17% of cases, patient can have symptoms in the other shoulder within 5 years (2).
Risk factors (3)
- Female (higher incidence compared to males)
- 40–59-year-olds
- Metabolic factors, such as diabetes, thyroid disorders & hyperlipidaemia
- Preceding trauma
- Prolonged immobilisation of the glenohumeral joint
- Other comorbidities, such as cerebrovascular disease, coronary artery disease, neurological conditions, autoimmune conditions, ankylosing spondylitis & Dupuytren’s disease.

Figure 4: Summary of clinic-based tests and characteristic clinical features
Community based assessment for frozen shoulder
- Primary care services may opt to utilise the local skillsets of first contact practitioners, with regards to corticosteroid injections and rehabilitation, to reduce waiting times.
- A multidisciplinary approach, with close links between MSK clinicians, Radiology, Orthopaedics and Pain services, can significantly improve patient outcomes and prognosis.
- Develop links between local shoulder orthopaedics teams for the early escalation of patients with rotator cuff tears following trauma.
- Shared decision making should be explored with patients, after counselling them on the natural history of resolution for frozen shoulder.
Is there a role for imaging?
Currently, the European Society of Musculoskeletal Radiology does not recommend the use of imaging to diagnose frozen shoulder (7).
| Advantages | Disadvantages | |
| MRI |
|
|
| Ultrasound |
|
|
Table 1: Imaging options for frozen shoulder (8,9)

Figure 5: MRI of a patient with frozen shoulder
Red arrow indicates pericapsular oedema in the axillary recess.
Although there are no existing diagnostic criteria for frozen shoulder, numerous studies have reported characteristic findings with MSK ultrasound. The presence of these findings, alongside a clinical history, can be useful in cases of diagnostic uncertainty.
The MSK ultrasound playbook for frozen shoulder
| Ultrasound findings | Sensitivity | Specificity | |
| Coracohumeral ligament thickening | – | – | |
| > 0.7mm (8) | 93.1 | 94.4 | |
| > 2.2mm (10) | 77 | 91.8 | |
| > 3mm (11,12) | 44.83-64.4 | 78.95-88.9 | |
| Increased soft tissue in the rotator interval (8,11,13) | 71.1-97 | 92.5-100 | |
| Axillary pouch thickening (5) | 100 | 98 | |
| > 2.0mm (14) | 100 | 96 | |
| > 3.5mm (11) | 93.3 | 66.7 | |
| > 4mm (5,10) | 68.9-93.4 | 90.2-98 | |
| < 4mm but > 60% vs contralateral side (5) | 6.6 | 98 | |
| Restricted external rotation of subscapularis
(dynamic scanning) (5,8) |
72.6-86.2 | 92.8-100.0 | |
| Bounce sign (5) | 41.5 | 100 | |
Table 2: Characteristic ultrasound findings
Point of care ultrasound (POCUS) enables US clinicians to rapidly assess for concurrent conditions and key differential diagnoses, such as rotator cuff tears, tendinopathies or bursitis, when there is diagnostic uncertainty.
POCUS also enables image-guided shoulder injections to be performed, which have shown to provide superior improvements in pain and shoulder functionality compared to blind injections (15). Ultrasound-guided hydro-distension and supra-scapular nerve block injections have also been shown to be effective in outpatients settings where expertise to deliver them are available (16,17).
Suprascapular Nerve & Notch:
Watch video here.
Infraspinatus Tendon
Watch video here.
Videos courtesy of : https://www.orcaresource.com
Post injection follow up; commence early rehabilitation to maximise the benefits of hydrodistension
Hydro-distension is a well-tolerated procedure and has a low risk of adverse events (18). It has shown to provide relief of symptoms in 93% of patients following their first hydro-distension procedure, with low rates of repeat interventions. To maximise the benefits of hydrodistension, an exercise programme should accompany the procedure. Self-directed, home exercise programmes following hydro-distension has shown to be as effective as supervised physiotherapy programmes (19).
Suprascapular nerve – to block or not to block?
Pain physicians, Sport & Exercise Medicine physicians, radiologists and orthopaedic surgeons regularly perform suprascapular nerve blocks (SSNB) for analgesia due to the sensory innervation of the subacromial bursa, posterior glenohumeral joint capsule and acromioclavicular joint.
A landmark technique or ultrasound guided technique can be used where the technical expertise is available. The aim of a SSNB is to improve the patient’s tolerance to hydrodistension, reduce pain during the procedure and after during physical therapy/ rehabilitation.
Dose: 5mls of 1% Lidocaine or 0.5% Bupivacaine/Levobupivacaine +/- Depomedrone
| Adjunctive therapy | Mechanism of action | Benefits |
| Hydrodistension (20–22) |
|
|
| Suprascapular nerve block (SSNB) (18) |
|
|
Table 3: Summary of the common adjunctive therapies

Figure 6: Summary of the post-treatment phase of the community based MSK pathway for frozen shoulder

Figure 7: Summary of what the community-based frozen shoulder pathways can offer
Conclusion
- Frozen shoulder remains a clinical diagnosis based on a patient’s history and examination.
- POCUS is typically used to exclude other causes of shoulder pain/stiffness, where there may be a clinical history (trauma or cuff tear) to suggest another diagnosis.
- Thickening of the coracohumeral ligament, increases in soft tissue in the rotator interval and axillary pouch thickening are characteristic ultrasound findings with good diagnostic accuracies.
- Suprascapular nerve blocks can be considered as an adjunct if the patient is unable to tolerate hydrodistension due to pain.
Authors and Affiliations: Rifat Hassan, Lynsey Abbey Joslin, Peter Resteghini, Hozefa Dahodwala, Dr Sadiq Bhayani, Dr Imran Lasker, Dr Irfan Ahmed, Mr Niel Kang
Rifat Hassan
Final Year Medical Student
University of Southampton
Twitter @RifatHassan_
Lynsey Abbey Joslin
Medical Student
University College London (UCL)
Twitter @AbbeyJoslin
Peter Resteghini
Consultant Physiotherapist & Musculoskeletal Sonographer
Course Director for the Postgraduate Certificate in Musculoskeletal Ultrasound (University of East London)
Homerton Hospital
@PeterResteghini
Hozefa Dahodwala
Advanced Practitioner Physiotherapist & Musculoskeletal Sonographer
Connect Health, United Kingdom
Twitter @Hozefa_Physio
Dr Sadiq Bhayani
Consultant Pain Physician
Cleveland Clinic Abu Dhabi, UAE
Founder Pain Flix
Co-Founder Gulf Pain School
Special interest in Ultrasound Guided Pain & MSK Interventional Pain Management
https://www.youtube.com/watch?v=aQSbzqoAmGU
Twitter @BhayaniSadiq
Dr Imran Lasker
Consultant Radiologist with Specialist interest in MSK
Mid & South Essex Foundation Trust
Twitter @DocLasker
Links to MSK/MRI courses: imranlasker.com, radiologyseminars.com. emergencyimaging.co.uk
Dr Irfan Ahmed
Locum Consultant in Musculoskeletal, Sport & Exercise Medicine
Addenbrookes Hospital
Twitter @ExerciseIrfan
Mr Niel Kang
Consultant Trauma & Orthopaedic Surgeon
Cambridge University Hospitals NHS Trust
Affiliate Assistant Professor
Clinical school of medicine, University of Cambridge
Education and Careers Committee
British Orthopaedic Association
Twitter @kangsta77
With thanks to:
Ultrasound video of the shoulder provided by Orca Resource & Peter Resteghini.
Orca Resource EdTech streaming platform provides a comprehensive series of high-quality videos for the medical industry including musculoskeletal ultrasound
No relevant conflicts of interests or relevant disclosures declared by any of the authors.