Keywords: Shoulder pain, diagnostic criteria, terminology
In this blog, we present the findings of our review mapping terminology and diagnostic criteria used in studies investigating subacromial pain syndrome (SAPS). We also provide our recommendations for planning future studies. The study was recently published in the BJSM.
Why is this study important?
If you are treating shoulder patients, you probably see many diagnosed with SAPS, shoulder impingement, and rotator cuff syndrome – or are they the same? It is important to have a common understanding of both terminology and diagnostic criteria to avoid confusion, communicate efficiently and navigate the literature.
SAPS is regarded as the most common cause of shoulder pain. Despite this, there is no universally recognised terminology or diagnostic criteria. An overview of trends in terminology can help us understand the ongoing discussion on the use of diagnostic labels, and aid communication among scientists and healthcare professionals. Differences in diagnostic criteria can foster misconceptions – if we do not agree on the definition of a problem, we cannot agree on the solution. To enable a qualified interpretation of the literature, it is important to have an overview and understanding of the terminology and diagnostic criteria used in the literature. You need to know the past to understand the present.
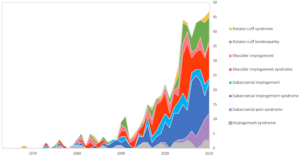
Figure 1: Terminology used in the period 1972–2019 to describe patients with subacromial pain syndrome.
How did the study go about this?
We did a comprehensive review, and mapped the terminology and the diagnostic criteria used in studies investigating SAPS.
What did the study find?
∙ The terminology used to describe patients with SAPS varies considerably across studies and time. More mechanistic terms containing ‘impingement’ are used less than before, while SAPS is used increasingly.
∙ The diagnostic criteria were often based on physical examination tests, but many studies did not report any diagnostic criteria. Combinations of Hawkin’s, Neer’s, Jobe’s, painful arc, injection test and isometric shoulder strength tests were most commonly used, though this varied considerably.
∙ Imaging was most often used to exclude other pathology, but it was not used consistently.
∙ Patients with full-thickness supraspinatus tears were often excluded, however, many studies did not report whether they included or excluded these patients.

Table 1: Physical examination tests and imaging modalities used to diagnose subacromial pain syndrome.
What are the key take-home points?
∙ Studies investigating SAPS are heterogeneous to an extent that makes it difficult, and often impossible, to compare studies.
∙ Future studies should have a clear definition of the patient population, and apply a systematic methodological approach, to ensure reproducibility and aid in the interpretation and generalisability of the findings.
∙ We recommend using the term SAPS. The word ‘subacromial pain’ encapsulates the cardinal symptom of SAPS, and the word ‘syndrome’ recognises that the pathophysiology is not fully understood.
∙ When classifying patients with SAPS, we recommend using a combination of physical examinations tests, and imaging, as other potential shoulder pathology, that can mimic the symptoms of SAPS, must be excluded. Common differential pathologies that must be excluded are glenohumeral osteoarthrosis, frozen shoulder, shoulder instability, full-thickness rotator cuff tears, neurological and cervical disorders.
∙ For research purposes, we recommend using standardized and protocolised physical examination tests in combination, such as the Hawkin’s, Neer’s, Jobe’s, painful arc, and external rotation resistance test, from which at least three must be positive, before patients can be classified as having SAPS.

References:
(1) Witten A, Mikkelsen K, Wagenblast Mayntzhusen T, et al Terminology and diagnostic criteria used in studies investigating patients with subacromial pain syndrome from 1972 to 2019: a scoping reviewBritish Journal of Sports Medicine Published Online First: 22 February 2023. doi: 10.1136/bjsports-2022-106340
Authors and affiliations:
Adam Witten 1, Karen Mikkelsen1, Thomas Wagenblast Mayntzhusen1, Mikkel Bek Clausen, Kristian Thorborg1, Per Hölmich1, Kristoffer Weisskirchneer Barfod1
1) IOC Research Center Copenhagen, Sports Orthopedic Research Center – Copenhagen (SORC-C), Arthroscopic Center, Department of Orthopedic Surgery, Copenhagen University Hospital, Amager-Hvidovre, Denmark
2) Department of Midwifery, Physiotherapy, Occupational Therapy and Psychomotor Therapy, Faculty of Health, University College Copenhagen, Copenhagen, Denmark