Keywords: athlete, diagnostic approach, lower airway dysfunction
This blog provides an overview of a recent study exploring lower airway dysfunction in athletes (1).
Why is this study important?
Lower airway dysfunction (LAD) is a collective term including exercise-induced asthma and/or exercise-induced bronchoconstriction and/or airway hyperresponsiveness; clinical definitions used interchangeably for symptoms suggestive of exercise-induced lower airway narrowing. This condition affects approximately one in five athletes.
A key challenge in this context, is that studies consistently demonstrate a poor relationship between presence of symptoms and objective evidence of exercise-induced lower airway narrowing in athletes. Hence, the Global Initiative for Asthma, (2) the International Olympic Committee – Medical Commission (IOC-MC) statements (3) and the World Anti-Doping Agency (4) strongly suggest that the LAD-diagnosis should include both LAD-symptoms and a positive objective bronchial provocation test (BPT) before eventual asthma treatment is initiated.
However, there is no gold standard BPT, and it is unclear which BPT would be the best diagnostic approach to confirm LAD.
How did the study go about this?
The aim of this work was to systematically review the available evidence comparing diagnostic test modalities in the context of
1) confirming a symptom-based diagnosis of LAD, and
2) screening for LAD in athletes, regardless of symptoms.
Hence, we included original full-text studies on 1) athletes / physically active individuals aged 15-65 years, who (2) had undergone assessment for LAD by symptom-based questionnaires/history and/or objective testing (i.e., direct or indirect BPT’s). Thereafter, a sensitivity and specificity meta-analysis was performed to compare test performance of the different BPTs.
What did the study find?
If your athlete has symptoms suggestive of LAD, this study demonstrates that field-based sport specific exercise challenge tests (ECT) and the eucapnic voluntary hyperpnoea (EVH) laboratory test, have moderate and similar test performances with a moderate specificity acceptable to rule in the LAD diagnosis.
In the context of screening your squad for LAD regardless of symptoms, this study demonstrates that field-based sport specific exercise challenge tests and the eucapnic voluntary hyperpnoea laboratory test, have moderate and similar test performances with a moderate sensitivity acceptable ability to rule out the LAD diagnosis.
What are the key take-home points?
In the assessment of LAD in athletes, field-based sport specific exercise challenge tests and the eucapnic voluntary hyperpnoea laboratory test, have moderate and similar test performances.
If the field-based sport specific exercise challenge test is performed at a high intensity level and in a cold environment, the sensitivity seems to be higher than that found for the eucapnic voluntary hyperpnoea test.
A BPT by inhaling provocative methacholine demonstrated a lower overall test performance.
The below infographic illustrates that in the case of a symptomatic athlete (on the left side), the eucapnic voluntary hyperpnoea laboratory test and field-based sport specific exercise challenge tests offer similar diagnostic test performance to rule in the LAD diagnosis, whilst if you screen your squad regardless of LAD symptoms (on the right side), these tests can be used to rule out the diagnosis.
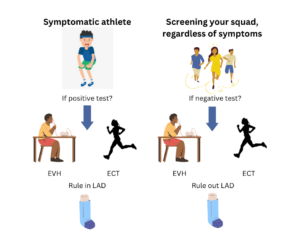
ECT – field-based sport specific exercise challenge test
EVH – eucapnic voluntary hyperpnoea laboratory test
LAD – lower airway dysfunction
References:
1: Reier-Nilsen T, Sewry N, Chenuel B, et al. Diagnostic approach to lower airway dysfunction in athletes: a systematic review and meta-analysis by a subgroup of the IOC consensus on ‘acute respiratory illness in the athlete’. British Journal of Sports Medicine 2023;57:481-489.
2: Asthma GIf. Global Strategy for Asthma Management and Prevention https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf2021 [
3: Fitch KD, Sue-Chu M, Anderson SD, Boulet L-P, Hancox RJ, McKenzie DC, et al. Asthma and the elite athlete: Summary of the International Olympic Committee’s Consensus Conference, Lausanne, Switzerland, January 22-24, 2008. J Allerg Clin Immunol. 2008;122(2):254-60.e7.
4: Anderson SD, Argyros GJ, Magnussen H, Holzer K. Provocation by eucapnic voluntary hyperpnoea to identify exercise induced bronchoconstriction. Br J Sports Med. 2001;35(5):344-7.
Authors and affiliations:
Tonje Reier-Nilsen (1,2), Nicola Sewry (3,4), Bruno Chenuel (5,6), Vibeke Backer (7,8), Kjell Larsson (9), Oliver J. Price (10,11), Lars Pedersen (12), Valérie Bougault (13), Martin Schwellnus (3,4), James H. Hull (14,15)
(1) The Norwegian Olympic Sports Centre, Norwegian Olympic and Paralympic Committee and Confederation of Sports ,Oslo, Norway
(2)Oslo Sports Trauma Research Center, Department of Sports Medicine, Norwegian School of Sport Sciences, Oslo, Norway
(3)Sport, Exercise Medicine and Lifestyle Institute (SEMLI), Faculty of Health Sciences, University of Pretoria, South Africa
(4)International Olympic Committee (IOC) Research Centre of South Africa, University of Pretoria, South Africa
(5)CHRU-Nancy, Department of Lung function and Exercise Physiology – University Center of Sports Medicine and Adapted Physical Activity, F-54000, Nancy, France
(6) Université de Lorraine, DevAH, F-54000 Nancy, France
(7) Department of ENT, Rigshospitalet, Copenhagen University, Denmark
(8) CFAS, Rigshopitalet, Copenhagen University, Denmark
(9) Integrative Toxicology, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden
(10) School of Biomedical Sciences, Faculty of Biological Sciences, University of Leeds, United Kingdom (UK)
(11) Leeds Institute of Medical Research at St. James’s, University of Leeds, Leeds, UK
(12) Department of Respiratory Medicine and Infectious Diseases, Bispebjerg Hospital, Copenhagen, Denmark
(13) Université Côte d’Azur, Laboratoire Motricité Humaine Expertise Sport Santé, Nice, France
(14) Department of Respiratory Medicine, Royal Brompton Hospital, London, UK
(15) Institute of Sport, Exercise and Health (ISEH), Division of surgery and Interventional science, University College London (UCL), London, UK