Is it being used out of proportion and how can we make it more effective?
Key words: Blue Card, Rugby, Concussion
Introduction
Rugby-related concussion has become one of the most controversial topics in sport, with many former professional players coming forward to discuss the long-term impacts concussion has had on their health and well-being. To mitigate these impacts the Blue Card (BC) initiative was set up and rolled out in 2014 to enable referees to remove players from play if they are suspected to have sustained a concussion(1). The BC continues to gain controversy among players, coaches, health professionals and referees.
The BC
The BC can be issued by a referee who has undergone specific training to identify concussion symptoms(1). If a referee suspects a player has sustained a concussion, they have the right to issue a BC(1). Following this decision, players are immediately removed from the field and undergo an immediate 21- or 23-day stand down depending on their age(1). The only exception is if an independent specialist medical doctor with expertise in the management of concussions provides clearance before this stand-down period ends(1). This process can take around 21 days resulting in players opting to complete the stand-down period instead. Players must follow a graduated return to play (GRTP) (Figure 1) and gain medical clearance from a General Practitioner (GP) before commencing Stage 5(1).
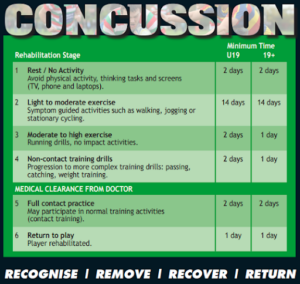
Figure 1 – Blue Card Concussion Initiative: Protocols and Implementation Procedures for Provincial Unions: Graduated Return to Play Protocol(1).
The BC and our struggling health system
Due to the current staffing crisis in health care across New Zealand, particularly in rural areas, GP appointments are limited, with some players waiting 5 weeks to see their GP(2). Unless a player presents to the emergency department, which is discouraged unless in an emergency, these players could wait 5 weeks for a confirmed medical diagnosis and clearance to play. Fortunately, New Zealand has concussion-trained physiotherapists, with many private practices having appointments available within 24-72 hours. Unfortunately, New Zealand physiotherapists are currently unable to medically diagnose a concussion. As a physiotherapist working in the private sector, with patients who are athletes, many GPs rely on my assessment to determine whether a player has sustained a concussion and assist them in clearing a player for contact training and return to play (RTP). Given the training and expertise of a physiotherapist with these specific skills, why is it they are unable to diagnose concussions and therefore, making decisions regarding their RTP. Changes to this system could assist extremely busy GPs.
Experiences with the BC
As a former rugby player and current sports physiotherapist, part of my role involves working with rugby teams, including side-line management during games. Given my clinical role and sporting history, concussion is an area of interest, in which I have upskilled. There are mixed opinions around the BC initiative. Although the intent is proactive and player welfare is a priority, there are questions around whether the training that the referees receive is appropriate. A recent study found that 72% of rugby referees felt they could subjectively diagnose a concussion based on reported symptoms but were not confident at recognising objective signs, with only 45% having received prior formalised concussion training (3).
Questions I have in this area
- Should physiotherapists be able to diagnose and provide clearance following a concussion?
- Should a BC be used if an appropriately qualified health professional is present and able to diagnose and manage a concussion?
- If being managed by an appropriately qualified health professional, should the stand-down timeframe apply, or should a symptom guided GRTP process be adopted?
What could be done differently?
- Referees only use the BC if no appropriately qualified health professional is present.
- Physiotherapists could complete specific training set by the Physiotherapy Board of New Zealand to become qualified to diagnose and clear a concussion.
Conclusion
The intent behind the BC is proactive and considers player welfare, however, in my opinion, is often overused and can significantly impact individuals who have not sustained a concussion. Allowing Physiotherapists to diagnose, manage and clear players who have sustained a concussion could assist to alleviate pressure on New Zealand’s health care system.

Authors name and affiliations
Bronwyn Prestage
Musculoskeletal and Sports Physiotherapist at Great Lake Physio, Taupo, New Zealand. She has completed her Post Graduate Certificate in Sports Physiotherapy through the School of Physiotherapy, University of Otago, New Zealand.
No conflicts of interest identified.
References
- New Zealand Rugby. Blue card concussion initiative: protocols and implementation procedures for provincial unions [Internet]. 2021 [updated 2021 May]; [cited 2022 Sep 15]. Available from: https://www.rugbytoolbox.co.nz/uploads/media/default/98/69/cb445c6f5f238406e72e350b8a92a13b69ad35ac.pdf?fbclid=IwAR3BLtbw3-MgPFcpXEky2QoVFxNxFsUY9WEW1bE1UCsindenFjVSydgAzrI.
- Salmon D, Sullivan J, Romanchuk J, et al. Infographic. New Zealand rugby’s community concussion initiative: keeping kiwi communities RugbySmart. Br J Sports Med. 2020;54(5):300-1. doi: 10.1136/bjsports-2019-100949 [accessed 2022 Sep 15].
- King C, Coughlan E. Blowing the whistle on concussion knowledge and education in youth sport referees. Open Access J Sports Med. 2021;12:109-17. doi: 10.2147/OAJSM.S324191 [accessed 2022 Sep 15].
- World Rugby. Head Injury Assessment (HIA) Protocol [Internet]. 2017 [updated 2017 Jul 3]; [cited 2022 Sep 15]. Available from: https://www.sareferees.com/uploads/files/Eugene%202017/180326%20HIA%20Protocol%20and%20Procedures.pdf.