Keywords: Body Mass Index, Lung, Physical fitness.
Introduction
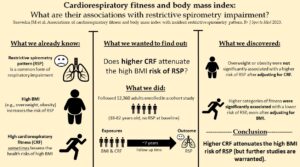
The role of the respiratory system is to move air in and out of the lungs to facilitate the process of gas exchange. Impairment of this system increases the likelihood of lung disease, a leading cause of death worldwide (1). Major risk factors of respiratory impairment include long-term exposure to tobacco smoke, older age, and high body mass index (BMI) (2). Restrictive spirometry pattern (RSP) is a common form of respiratory impairment that significantly increases the risk of death (3). RSP is characterized by a reduced lung volume and is exacerbated by high BMI (4). Cardiorespiratory fitness (CRF) reflects the body’s ability to efficiently transport and utilize oxygen, and greater CRF is associated with lower risks of obesity-related diseases like cardiovascular disease (CVD) (5). However, little is known about the influence of CRF on RSP risk in the general population, either independently or combined with BMI.
This blog is based on the paper recently published in the BJSM.
Why is this study important?
Approximately 35-50% of the population in high income countries will be obese by 2040 (6,7). Therefore, the prevalence of RSP and the increased risk of death associated with it will likely worsen with time. Understanding the role played by CRF and its interaction with BMI on the development of RSP will likely provide health professionals with additional tools to combat the growing burden of respiratory impairment in the general population, potentially offsetting the long-term risks of chronic lung disease and mortality. Furthermore, there is a scarcity of public health recommendations for the prevention of lung disease beyond tobacco smoke cessation and body weight loss, behaviors that many people find difficult to sustain long-term (8,9). This study is important because it examines how the risk of RSP is influenced by both BMI and CRF; the latter of which is modifiable without necessarily losing weight (10)
How did the study go about this?
We conducted an observational study using data from the Aerobic Centre Longitudinal Study (ACLS), (11) which is a large cohort of individuals who attended the Cooper Clinic (Dallas, TX) between 1974-2003 to undergo preventative medical examinations. We evaluated CRF using a treadmill test and BMI using weight (kg) divided by the square of height (m) among 12,360 adults (18-82 years) who were free from RSP at baseline. We followed these individuals over an average period of 7 years and calculated the risk of developing RSP (measured by spirometry) as a function of:
1) categories of CRF,
2) categories of BMI,
3) joint categories of CRF/BMI (fit-fat analysis).
What did the study find?
Compared to those in the lowest fitness category, those in the highest fitness category had a 41% lower risk of RSP after adjusting for confounders (including BMI). Compared to normal weight (BMI <25kg/m2), those classed as obese (BMI ≥30.0 kg/m2) had a 30% higher risk of RSP after adjusting for confounders. However, this risk was reduced when we additionally adjusted for CRF. As shown in Figure 1, when examining the associations among combinations of CRF and BMI categories, the risk of RSP was 23%-30% lower for ‘fit’ individuals regardless of their baseline BMI category.
What are the key take-home points?
We found that higher levels of CRF, independent of BMI, were associated with lower risks of RSP. We also found that obesity was associated with a higher risk of RSP, but this risk was negated when accounting for CRF. In our joint analysis, fitter individuals (regardless of BMI status) had lower risks of RSP, with those deemed ‘fit and normal weight’ having the lowest risk of all groups. These findings suggest that higher CRF is associated with a reduced risk of RSP, regardless of BMI. Because this study was observational, future studies are needed to determine if improving CRF reduces the risk of developing RSP. Physical activity, which can increase CRF, should be considered in future public health studies as it may promote lung health alone or in combination with standard weight-related guidance.
Authors: Saavedra JM, Brellenthin AG, Song BK, Lee DC, Sui X, Blair SN.
References:
1 Mannino DM, Buist AS, Petty TL, Enright PL, Redd SC. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow up study. Thorax. 2003;58(5):388-393. doi:10.1136/thorax.58.5.388.
2 Bui DS, Perret JL, Walters EH, et al. Lifetime Risk Factors for Pre- and Post-Bronchodilator Lung Function Decline. A Population-based Study. Ann Am Thorac Soc. 2020;17(3):302-312. doi:10.1513/AnnalsATS.201904-329OC.
3 Guerra S, Sherrill DL, Venker C, Ceccato CM, Halonen M, Martinez FD. Morbidity and mortality associated with the restrictive spirometric pattern: a longitudinal study. Thorax. 2010;65(6):499-504. doi:10.1136/thx.2009.126052.
4 Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018;12(9):755-767. doi:10.1080/17476348.2018.1506331.
5 Kaminsky LA, Arena R, Ellingsen Ø, et al. Cardiorespiratory fitness and cardiovascular disease – The past, present, and future. Prog Cardiovasc Dis. 2019;62(2):86-93. doi:10.1016/j.pcad.2019.01.002.
6 Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440–50.
7 Cancer Research UK. New analysis estimates over 21 million UK adults will be obese by 2040. Available: https://tinyurl.com/5a5rzp8x [Accessed July 2022].
8 Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6(6):e011045. Published 2016 Jun 9. doi:10.1136/bmjopen-2016-011045.
9 Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S-225S. doi:10.1093/ajcn/82.1.222S.
10 Simati S, Kokkinos A, Dalamaga M, Argyrakopoulou G. Obesity Paradox: Fact or Fiction? Curr Obes Rep. 2023;10.1007/s13679-023-00497-1. doi:10.1007/s13679-023-00497-1.
11 Blair SN, Kohl HW 3rd, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395-2401. doi:10.1001/jama.262.17.2395.
12 Burtscher J, Millet GP, Gatterer H, Vonbank K, Burtscher M. Does Regular Physical Activity Mitigate the Age-Associated Decline in Pulmonary Function? Sports Med. 2022;52(5):963-970. doi:10.1007/s40279-022-01652-9.