Motivational Interviewing – A new way of fostering behaviour change.
What is motivational interviewing?
Motivational Interviewing (MI) is a communication style placing emphasis on compassion, acceptance, partnership, and evocation. Together these elements form the foundation or “spirit” of MI (1). It frames the conversation in a collaborative manner with the intention of enhancing an individual’s intrinsic motivation and commitment to change (2). Within this framework there is a focus on affirmative language emphasizing strengths demonstrated by the patient.
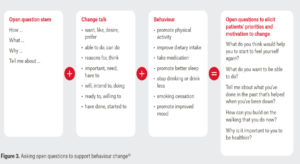
* Above figure provides some examples of open-ended questions used in MI
Figure taken from (6), with permission.
Applicability to Sports Physiotherapy:
Injuries are a common occurrence in the sporting environment. They result in a loss of playing time and impact team dynamics dramatically. As physiotherapists dealing with injured athletes, we are often presented with a degree of resistance when offering advice.
These include but are not limited to the following statements:
- “I just don’t have time to do my exercises”,
- “I know how important sleep is, but I just can’t see myself getting anymore”
- “Between training and my other commitments, it doesn’t leave room for much else”
- “I want to get back to playing, but I’m scared of injuring myself again”
Working in this environment, physiotherapists tend to place the blame of poor adherence on the athlete. This leads to further resistance from the athlete and subsequent frustration for physiotherapists, who feel a large degree of responsibility for the promotion of behaviour and lifestyle changes. This may result in miscommunication, preventing trust and rapport being established between the clinician and athlete. Distrust and disengagement can negatively impact the patient/therapist relationship, potentially leading to the athlete withholding information about their injury or condition.
Improving the Therapist/Athlete relationship:
Often there is an evident imbalance in the therapist/athlete relationship, with the therapist assuming an authoritative role and minimal autonomy given to the patient in the clinical decision-making process. In recent years there has been a shift in the way physiotherapists communicate with patients. Evidence has shown that effective communication skills are essential to patient care in athletic training and rehabilitation (3). Injured athletes often deal with a variety of psychological factors restricting their return to pre-injury performance (4). Factors such as maladaptive views about their injury, worry regarding prolonged loss of playing, and stress related to a perceived lack of competence can create barriers to the rehabilitation process. Recovery from physical pain and emotional distress, resulting from injury, requires the support of a trusted physiotherapist working in collaboration with the athlete towards a common goal. These impediments can be overcome through practitioner empathy and understanding, resulting in more comprehensive rehabilitation. One way this is achieved is through the use of a communication technique known as MI. Theoretically, MI strengthens the therapeutic relationship between the patient and therapist, which has been linked to improved rehabilitation results (5, 6). A collaborative approach between all those engaged in the athlete’s care is advocated, rather than one favouring a more dictated approach in which the patient is the passive recipient of therapist instructions. Utilizing MI encourages shared clinical decision making between the therapist, team management and athlete, allowing for the provision of holistic athlete care. Although MI has been examined from a physiotherapy perspective, other team personnel such as the Coach, Team Physician, and Exercise Physiologist may find MI of significant value.
Integration into Clinical Practice:
Working as a side-line rugby physiotherapist a number of years ago, I commonly used authoritative communication approaches when addressing players. Overall, there was a lack of compassion and understanding when players failed to meet expected requirements. Reasons for non-adherence were not tolerated, and players were blamed for being “lazy”, showing a lack of commitment, or “not wanting it enough”. Integrating MI into my clinical practice has been invaluable, I now view patients as being ambivalent, rather than non-adherent or lacking effort. Complex and difficult conversations with athletes have become significantly less strenuous to navigate, while subsequently dealing with any perceived resistance in a non-confrontational way. It has resulted in a higher level of job satisfaction and a marked decline in compassion fatigue.
Take home message:
MI promotes a focus on the athlete’s strengths, while increasing internal motivation for behaviour change. Through collaboration and recognition of autonomy, the athlete has the opportunity to actively participate in their rehabilitation.

Authors:
Denzil Jewell (BHsc Phty) – Physiotherapist at Hillcrest Physiotherapy in Hamilton. Recently completed a Post Graduate Diploma in Health Science, majoring in Musculoskeletal Management.
References:
- McKenzie KJ, Pierce D, Gunn JM. Guiding patients through complexity: Motivational interviewing for patients with multimorbidity. Aust J Gen Pract. 2018;47(1-2):8-13.
- Resnicow K, McMaster F. Motivational Interviewing: moving from why to how with autonomy support. Int J Behav Nutr Phys Act. 2012;9:19.
- Covassin T, Beidler E, Ostrowski J, Wallace J. Psychosocial aspects of rehabilitation in sports. Clinics in sports medicine. 2015;34(2):199-212.
- Podlog L, Dimmock J, Miller J. A review of return to sport concerns following injury rehabilitation: practitioner strategies for enhancing recovery outcomes. Phys Ther Sport. 2011;12(1):36-42.
- Howick J, Moscrop A, Mebius A, Fanshawe TR, Lewith G, Bishop FL, et al. Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis. J R Soc Med. 2018;111(7):240-52.
- Fuentes J, Armijo-Olivo S, Funabashi M, Miciak M, Dick B, Warren S, et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther. 2014;94(4):477-89.