What’s new for female hormone health?
At the start of the year, the National Institute for Health and Care Excellence (NICE) in the Clinical Knowledge Summaries (CKS) updated the guidelines for the management of bone health in the situation of amenorrhoea with low oestrogen. Hormone replacement therapy (HRT) is advised, rather than the combined oral contraceptive pill (COCP)[[1]]. This update is particularly relevant for female exercisers, athlete and dancers presenting with functional hypothalamic amenorrhoea (FHA) where the underlying cause is relative energy deficiency in sport (RED-S)[[2]]. Pharmaceutical bone protection with transdermal HRT is in keeping with Endocrine Society guidelines[[3]] and the International Olympic Committee (IOC) consensus statements on RED-S[2].
Importance of female hormone health
Why is this update so important? Female hormones are not just about reproduction. These hormones support many aspects of physical and mental health. Oestrogen is the protagonist when it comes to mediating the multisystem beneficial effects on the musculoskeletal, cardiovascular and neurological systems[[4]]. So, where amenorrhoea is accompanied by low levels of oestrogen it is essential to address the underlying cause and consider providing temporising oestrogen replacement. The COCP does neither.
Combined oral contraceptive pill: the good, bad and the ugly
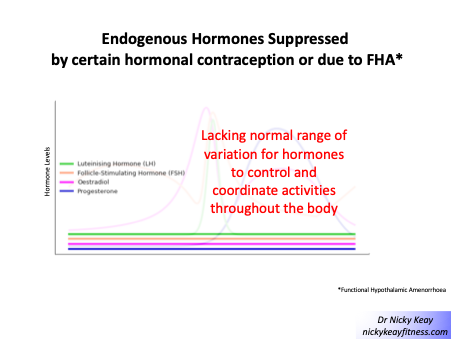
The COCP is an effective hormonal contraception. The mechanism of action is the suppression of the hypothalamic-pituitary axis. This can be seen on blood testing where low levels of follicle stimulating hormone (FSH), luteinising hormone (LH) oestradiol and progesterone are found. This is also precisely the pattern seen in FHA. In other words, the COCP acts as a masking agent of internal hormone function, reinforcing and maintaining the hormone suppression pattern of FHA. This is shown in the figure of suppressed of endogenous female hormones due to hypothalamic suppression found in FHA and from hormonal contraception use (COCP and also certain progestone contraception preparations).
The COCP induces a withdrawal bleed which may give a psychological boost to the athlete with FHA and her prescribing doctor. However, this is not a menstrual period, as it is not the result of internal hormone function. Although exogenous non-body identical oestrogen, ethynyl oestradiol, found in most forms of COCP may “fool” the hypothalamus-pituitary and the endometrium, this is not the case either for the specific assay for endogenous 17β-oestradiol, nor for bone. In FHA, the COCP does not have any bone protective effect compared to HRT which does have a beneficial effect on bone health[[5]]. This is also the case for women with amenorrhoea due to POI (primary ovarian insufficiency) where the British Menopause Society advise that HRT is more beneficial in improving bone health and cardiovascular markers compared to the COCP containing ethynyl oestradiol[[6]].
HRT to the rescue
In terms of the type of HRT, the most favourable is transdermal oestradiol (patch or gel) with cyclical body identical micronised progesterone. The transdermal route of 17β-oestradiol avoids the first pass effect of being metabolised in the liver. Furthermore, the purpose of HRT is replacement to physiological levels, rather than suppression of internal production with the COCP. However, women should be advised that HRT is not a contraceptive and so non-hormonal, barrier methods should be used if contraception is required[3].
Female hormone health in RED-S
It is also important to discuss with the athlete experiencing FHA due to RED-S, that HRT is a temporising step to protect bone health. It is essential to strive to restore energy availability and endocrine function for long term health and athletic performance. FHA is reversible with appropriate behavioural changes around nutrition and training load. This will often require medical, dietetic and psychological support, with contributions from coach and physiotherapist where indicated[[7]].
Amenorrhoea is a clinical sign
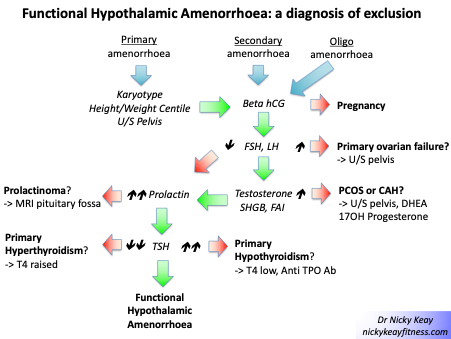
Another important point is that amenorrhoea is a clinical sign, not a diagnosis. Amenorrhoea is a situation of lack of periods. This can be primary amenorrhoea, where periods have not established by 16 years of age. Or secondary amenorrhoea, where periods have stopped for 6 months or more, in a previously regularly menstruating woman. Depending on the cause of amenorrhoea, oestrogen levels will not necessarily be low. So as a starting point it is essential to establish the cause of amenorrhoea to direct appropriate management.
The figure shows the pathway to follow to identify the cause of amenorrhoea. In any woman presenting with amenorrhoea, pregnancy, a physiological cause of amenorrhoea, must be excluded. After excluding pregnancy, the cause of amenorrhoea is identified based on FSH and LH levels. Raised FSH and LH in the presence of low oestrogen suggests primary ovarian insufficiency (POI) and treatment with HRT is indicated. Where FSH and LH are not unduly raised and oestrogen is in range, or raised; in the presence of elevated testosterone, this is suggestive of polycystic ovary syndrome (PCOS). Where FSH and LH are low range, together with low range oestradiol prolactin should be scrutinised to exclude prolactinoma as the cause of hypothalamic amenorrhoea (HA). Before settling on a diagnosis of FHA, other endocrine causes of amenorrhea should be considered, such as thyroid disorders. FHA is a diagnosis of exclusion[[8]].
Conclusions
Female hormone disruption due to RED-S, can produce adverse effects on health and performance. Therefore, early identification of those individuals at risk is an important prevention strategy[[9]]. New approaches including application of artificial intelligence techniques to model female hormones are being explored[[10]]. For a female athlete presenting with amenorrhoea, directed investigation is required to confirm FHA. The priority is to provide the athlete with support to change behaviours to restore hormone health. For bone protection during this restorative process, updated NICE guidelines advise treatment with HRT.
Author: Dr Nicky Keay, Honorary Clinical Lecturer UCL
References
[1] National Institute for Health and Care Excellence (NICE) Clinical Knowledge Summaries (CKS) Managing risk of osteoporosis (primary and secondary amenorrhoea) 2022 https://cks.nice.org.uk/topics/amenorrhoea/management/secondary-amenorrhoea/#managing-osteoporosis-risk
[2] Mountjoy M, Sundgot-Borgen JK, Burke LM, et al IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update British Journal of Sports Medicine 2018;52:687-697.
[3] Gordon C, Ackerman K, Berga S et al, Functional Hypothalamic Amenorrhea: An Endocrine Society Clinical Practice Guideline, The Journal of Clinical Endocrinology & Metabolism, 2017, 102 (5): 1413–1439, https://doi.org/10.1210/jc.2017-00131
[4] Keay N. What’s so good about Menstrual Cycles? British Journal of Sports Medicine 2019 https://blogs.bmj.com/bjsm/2019/02/08/whats-so-good-about-menstrual-cycles/
[5] Ackerman KE, Singhal V, Baskaran C, et al Oestrogen replacement improves bone mineral density in oligo-amenorrhoeic athletes: a randomised clinical trial British Journal of Sports Medicine 2019;53:229-236.
[6] British Menopause Society https://thebms.org.uk/publications/consensus-statements/premature-ovarian-insufficiency/
[7] Keay N. Returning to Sport/Dance restoring Energy Availability in RED-S? British Journal of Sports Medicine 2019 https://blogs.bmj.com/bjsm/2019/03/26/returning-to-sport-dance-restoring-energy-availability-in-red-s/
[8] McCarthy O, Pitt J, Keay N et al Passing on the exercise baton: what can endocrine patients learn from elite athletes? Clinical Endocrinology 2022 https://onlinelibrary.wiley.com/doi/10.1111/cen.14683
[9] British Association of Sport and Exercise Medicine educational website on RED-S www.health4performance.co.uk
[10] Keay N. Hormone Intelligence for Female Dancers, Athletes and Exercisers British Journal of Sports Medicine 2019 https://blogs.bmj.com/bjsm/2021/06/28/hormone-intelligence-for-female-dancers-athletes-and-exercisers/