Part of the BJSM’s Knowledge Translation blog series
In this blog we will explain how we used data from the Coronary Artery Risk Development in Young Adults (CARDIA) study to investigate the association between physical activity (PA) and coronary artery calcium progression and subsequent cardiovascular disease events. More details are available in our recently published manuscript in BJSM (https://bjsm.bmj.com/content/early/2022/03/13/bjsports-2021-105092).
Why is this study important?
It is recommended that healthy adults should perform a minimum of 150 min of moderate-intensity exercise or 75 min of vigorous-intensity exercise weekly. However, there is growing concern that excessive exercise, such as that undertaken by endurance athletes, may be deleterious to cardiovascular health. Several studies suggested a U- or reverse J-shaped dose-response relationship between lifetime PA exposure and cardiovascular morbidity, indicating that there is an exercise threshold beyond which some of the aforementioned cardiovascular benefits of PA are lost.
Coronary artery calcium (CAC) is a strong predictor of cardiovascular morbidity and mortality and a potent CVD risk stratification tool. Studies based on only a single measure of self-reported PA showed discordant cross-sectional association between PA and CAC during the past decades.
This study is important as we collected at least 3 PA measurements prior to follow-up CAC and determined PA trajectories, which can better reflect habitual PA of each individual. We evaluated the association between PA trajectories and CAC progression and subsequent cardiovascular disease (CVD) events among the same cohort, so as to comprehensively investigate the role of different PA levels in coronary atherosclerosis.
How did the study go about this?
A total of 2497 participants with 1120 (44.9%) male and 1418 (56.8%) white were eligible for the analysis. Self-reported PA was assessed with the validated CARDIA Physical Activity History questionnaire. PA trajectory groups were identified by using latent class models. CAC was measured by computed tomography with the Agatston scores, and CAC progression was defined as CAC>0 at follow-up for participants with CAC=0 at baseline; and an annualized change of 10 or percent change of ≥10% for those with 0<CAC<100 or CAC≥100 at baseline, respectively. The incident CVD events contained fatal and non-fatal coronary heart disease, hospitalization for heart failure, stroke, transient ischemic attack, or intervention for peripheral artery disease.
What did the study find?
Three distinct PA trajectory groups were identified: low PA trajectory (n=1332, 53.3%), below PA guidelines. moderate PA trajectory (n=919, 36.8%), meeting and slightly over PA guidelines. high PA trajectory (n=246, 9.9%), about 3 times PA guidelines or more (Figure 1). During a mean (SD) follow-up of 8.9 (2.1) years, 640 (25.6%) participants had CAC progression. The prevalence of CAC progression was 321 (24.1%), 235 (25.6%), and 84 (34.1%) in the low, moderate, and high PA trajectory groups, respectively. Compared with the low PA trajectory, high PA trajectory had a higher risk of CAC progression (adj. HR 1.51; 95% CI: 1.18-1.94).
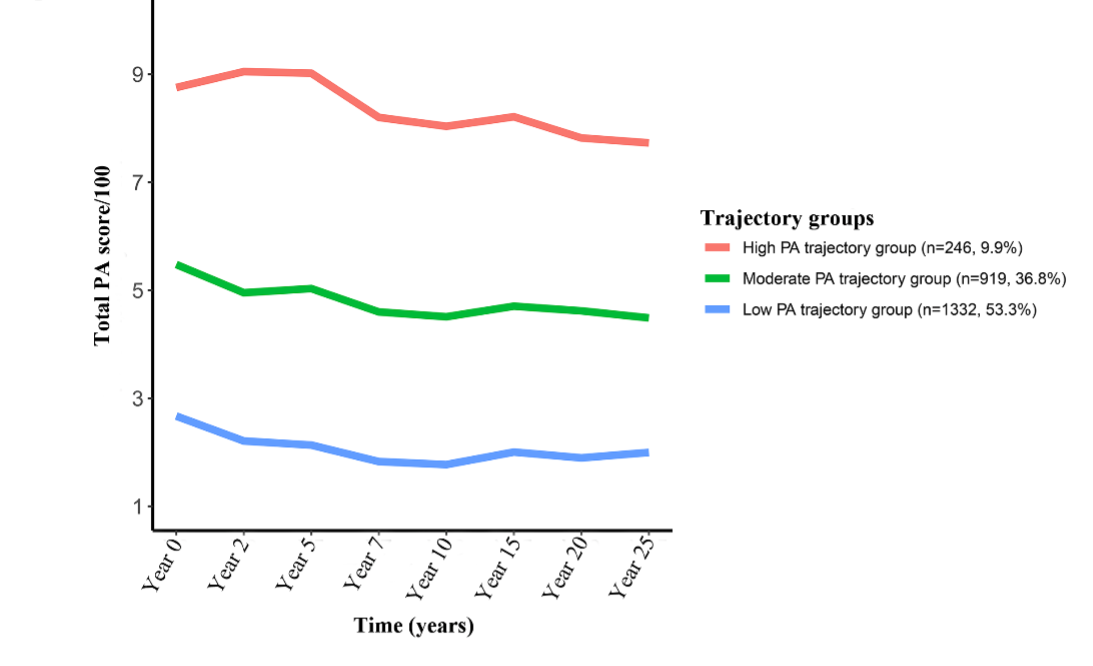
Figure 1. Trajectories of physical activity (PA) over 25 years.
After a subsequent mean (SD) follow-up of 6.9 (2.1) years, a significantly higher incidence of CVD events was observed in participants with CAC progression than in those without among all 3 PA trajectory groups (27/321 [8.4%] vs 8/1011 [0.8%], 20/235 [8.5%] vs 3/684 [0.4%], and 5/84 [6.0%] vs 2/162 [1.2%] in the low, moderate and high PA trajectory group, respectively, all P<0.05). However, the incidence of CVD events in participants with CAC progression was identical across all 3 PA trajectory groups (P=0.736, Figure 2).
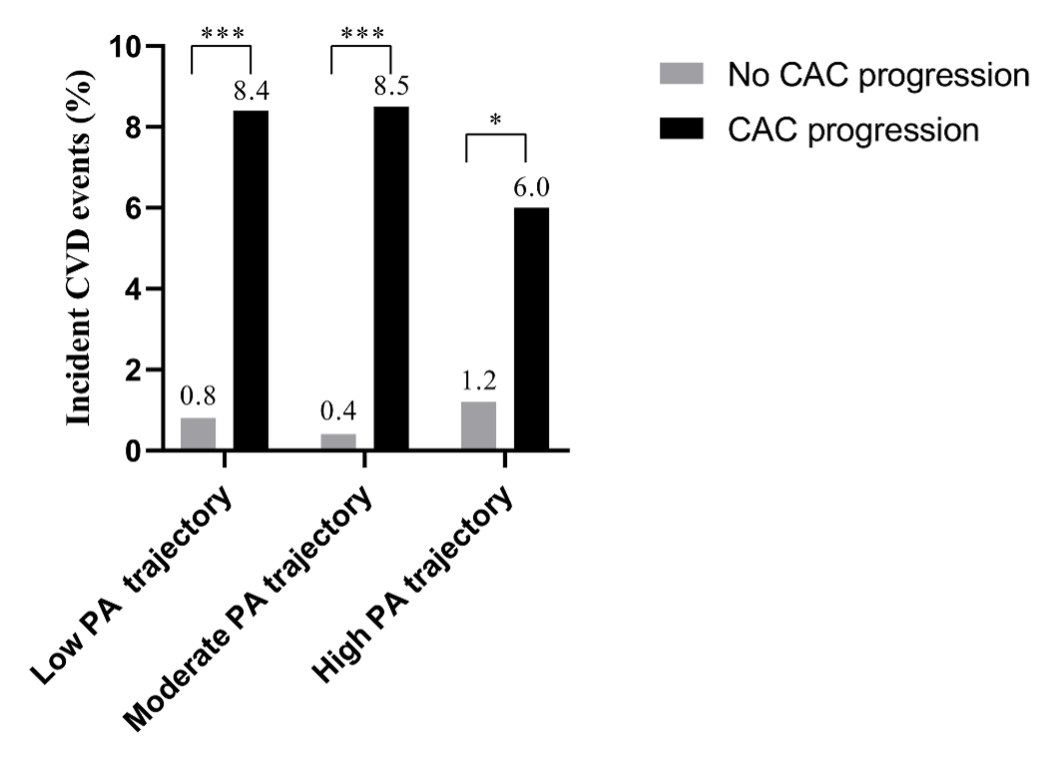
Figure 2. Incidence of CVD events per PA trajectories stratified by CAC progression status.
What are the key take-home points?
In the general population, as is suggested in professional athletes, high volumes of PA are independently associated with CAC progression, while no increased cardiovascular risk could be detected, which may represent a clinically benign phenotype. While CAC screening can add to a comprehensive CVD risk assessment in adults, CAC scores should be interpreted along with conventional risk factors for CVD and possibly PA levels. More research is needed to guide interpretation of CAC screening in adults with high PA.
Author and Affiliation:
LIU Pin-Ming, MD, PhD
Professor of Medline
Department of Cardiology,
Sun Yat-sen Memorial Hospital,
Sun Yat-sen University,
107 Yanjiang W Rd, Guangzhou 510120, China