In this blog we will explain how we used two concepts to develop an exertional heat stroke prediction tool. Our study (recently published in BJSM) took more than two years to complete and was collaboration between three U.S. Army organizations: U.S. Army Research Institute of Environmental Medicine (USARIEM), U.S. Army Medical and Material Development Agency (USAMMDA); and the Martin Army Community Hospital (MACH), Ft. Benning GA; and the Massachusetts Institute of Technology – Lincoln Laboratory (MIT-LL).
Why is this study important?
Exertional heat stroke (EHS) is a life threatening illness in which exercise, environment, clothing, and other factors combine to produce a rapid and abnormal increase in body core temperature – often higher than 40.5 °C – and central nervous system (CNS) dysfunction that can often be noticed as wobble (ataxia) in an athlete/Soldier’s movement.

While advances have been made in environmental monitoring and managing environmental risk (high temperatures, and high humidity) EHS remains a problem for many high intensity activities with heat strokes still occurring during military training and athletic events. Many cases can also occur in temperate or cool conditions, often among fit individuals with a high motivation to complete a task or event. Rapid cooling within minutes is essential to halt progression of the disease, prevent neurological damage, and improve clinical outcomes.
This study is important as we collected physiological and biomechanical measurements from six volunteers prior to and post collapse from EHS. To capture these data we collected over 3400 examples of high intensity runs and timed ruck marches from over 1800 individuals. We thought that high core body temperatures combined with a wobble in movement could be observed prior to collapse using a fairly simple wearable sensing technology.
How did the study go about this?
We used a new prototype chest belt monitor called the Heat Illness Prevention System (HIPS) (ODIC, Littleton MA) developed by USAMMDA. The device measures heart rate, skin temperature, and movement by accelerometry, and can record data for seven consecutive days. The simplicity of these devices let us instrument large classes of military trainees and record data from their high intensity training across multiple days (see figure below). Trainees who experienced heat illnesses were assessed by medical staff, cooled by ice-sheets, and transported by ambulance to the emergency department.
What did the study find?
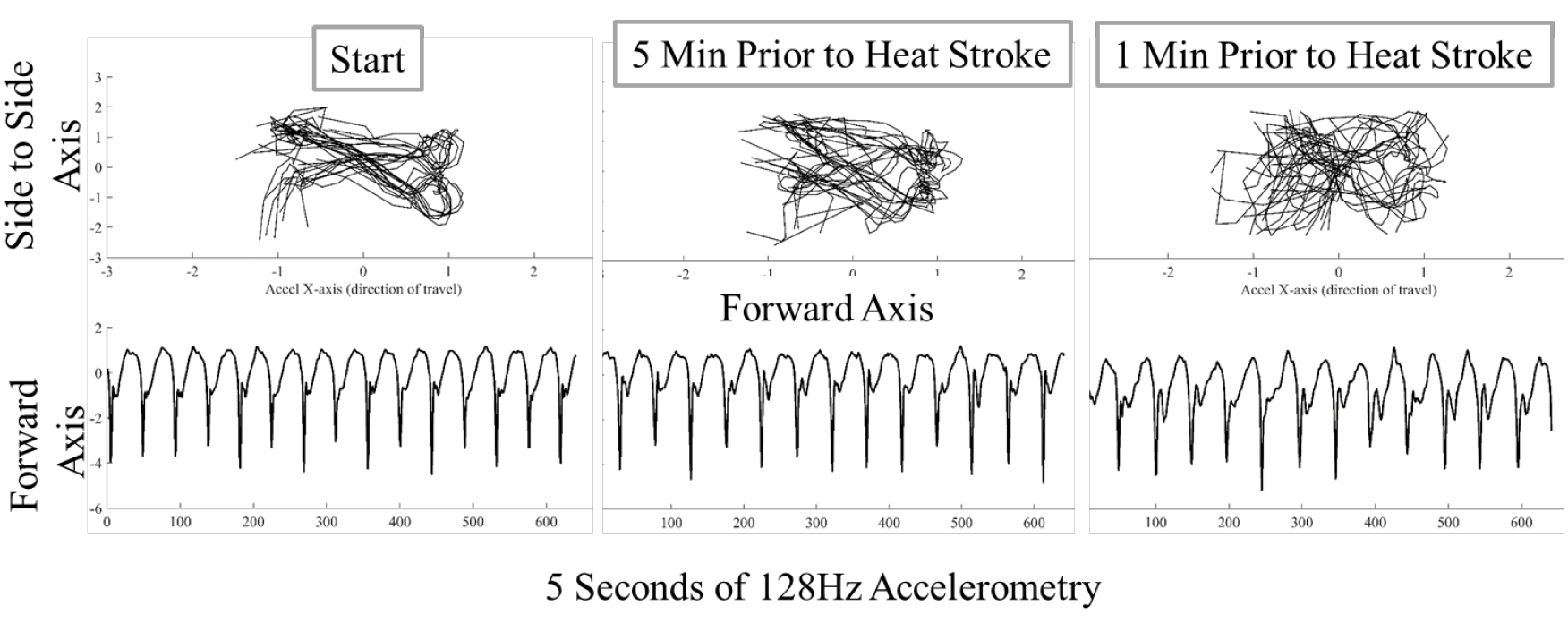
We found that individuals who experienced a heat stroke began to demonstrate ataxia – wobble in their movement patterns – that became more pronounced closer to the point of collapse. This pattern can be observed in the figure below. Each plot below depicts data from an accelerometer showing ~14 steps within five second windows. At the start of the run the student shows a regular movement pattern that becomes successively less regular at five minutes and one minute prior to collapse from heat stroke.
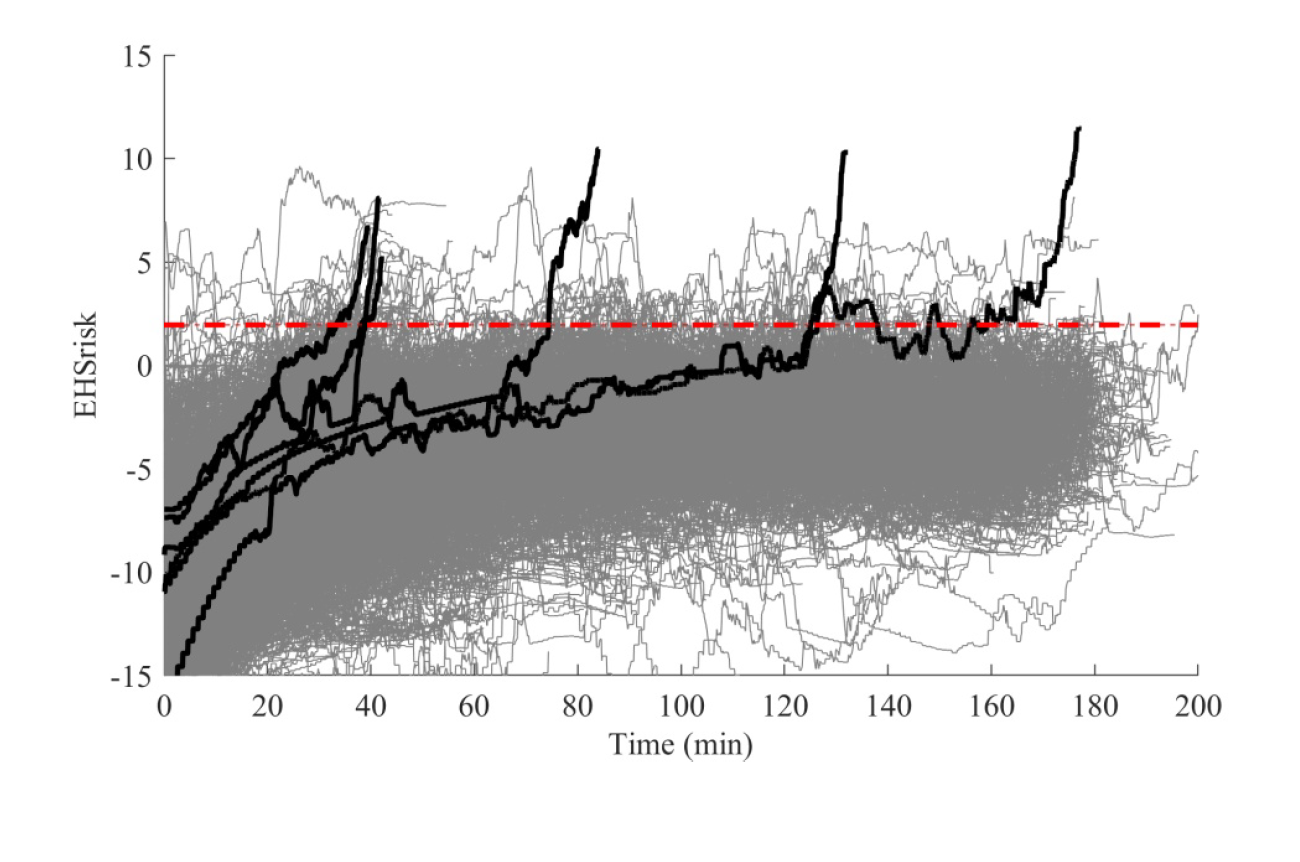
Using wobble detection and combing this with an accurate heart rate based estimate of core body temperature, we found we could predict all six heat stroke cases at least 3.5 minutes in advance of collapse with only a 6.1% false positive rate. This low false positive rate makes it possible to quickly direct training staff to an individual for face-to-face assessment in real time. Rather than responding after the fact, this system predicts imminent heat stroke and allows for early assessment and intervention prior to collapse. The figure below shows our combined estimated temperature and movement wobble score for all 3422 events showing the heat stroke casualties in black and our alerting threshold.
What are the key take-home points?
Using just heart rate and accelerometry, two algorithms can predict heat stroke at least 3.5 minutes in advance with a low false positive rate. These measures are fairly common on most modern sports physiological sensors. Applying these algorithms can make heat stroke assessment proactive versus reactive, and prevent athletes from progressing into life-threatening heat stroke.
Author and Affiliations:
Mark Buller, Max Bursey, Meghan Galer
Dr Mark Buller, United States Army Research Institute of Environmental Medicine, Natick, MA 01516, USA