What are the changes from #Tokyo2020?
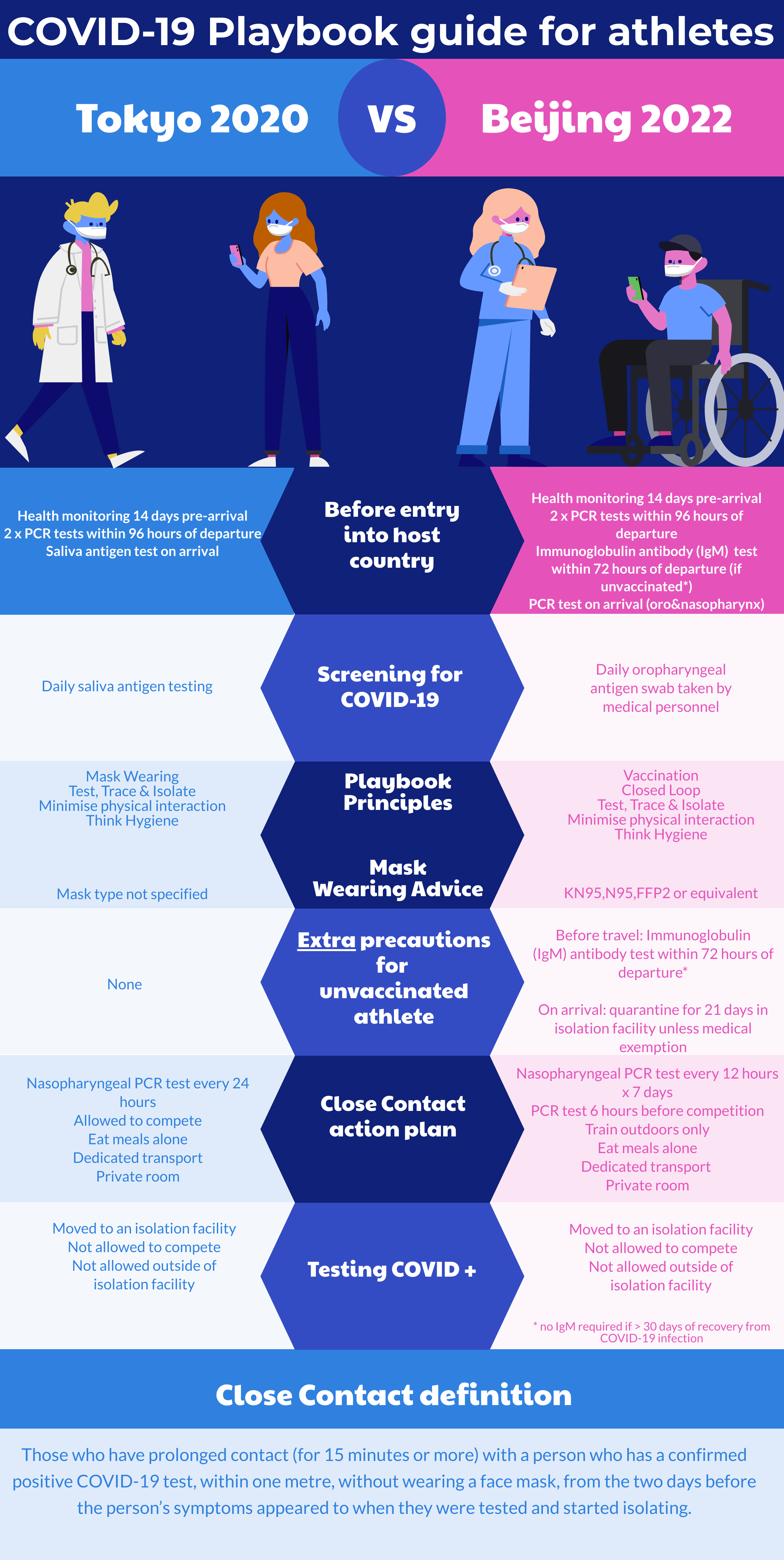
Despite being held six months apart, there are significant differences between Tokyo 2020 and Beijing 2022 COVID-19 screening and vaccination policies. The changes likely reflect current COVID-19 trends globally and differences in host nation policies.
Vaccination guidelines for Beijing 2022
- The emergence of the COVID-19 omicron variant has seen a return to disruptions and restrictions of elite sporting fixtures.
- The Beijing 2022 Winter Olympics and Paralympics (beginning in February and March 2022 respectively) issued the final version of its playbook in December 2021.
- This Playbook was developed by the International Olympic Committee, the International Paralympic Committee and the Beijing 2022 organising committee in collaboration with the Chinese government and local authorities [1].
- The Playbook advises that in order to enter the Olympic Village, athletes must be fully vaccinated at least 14 days prior to departure for China or undergo a 21 day quarantine period in Beijing, unless medically exempt [1].
- The Beijing 2022 protocols for vaccination of athletes seem new for an Olympics despite calls to have them previously.
- An influenza outbreak at the Calgary Winter Olympics in 1988 prompted physicians to seek mandatory vaccination prior to future games [2]. Further outbreaks occurred at both the Nagano and Salt Lake City Winter Olympics in 1998 and 2002 respectively [3].
- At Tokyo 2020, while preventative advice was given, no documentation of COVID-19 vaccination status was required for athletes to enter the Olympic village [4].
- Tokyo 2020 had relatively low rates of COVID-19 infection with just 33 athletes testing positive amongst a total of 11,300 competitors [5].
- Early data on the omicron variant suggests a higher transmissibility and vaccine breakthrough rate [6].
COVID-19 screening for athletes – Beijing 2022 vs. Tokyo 2020
- Differences in COVID-19 screening between Beijing 2022 and Tokyo 2020 are evident [1][4] and reflect host country policy.
- At Beijing 2022, unvaccinated athletes will require an immunoglobulin antibody (IgM) test pre-arrival*. This was not required for Tokyo 2020.
- Other differences in COVID-19 prevention include mask type and close contact action planning. (see infographic)
Athlete Risk
- The specific risk that COVID-19 poses to athletes is difficult to quantify and is likely multifactorial in aetiology.
- Global travel and mass congregation can increase the risk of viral transfer for athletes [7][8].
- The systemic response to high intensity exercise; release of cortisol coupled with high levels of circulating proinflammatory cytokines can result in an “open window” when an athlete is susceptible to infection [9].
- Athletes with COVID-19 infection follow graduated return to play guidelines [10].
- Little data exists on long-COVID in the elite athlete population and the ability to return to pre-COVID levels of activity.
Athlete attitudes & vaccine side effects
- Vaccine hesitancy amongst the elite athlete population has been previously documented.
- Fear of potential side effects affecting athlete performance, missing training time following vaccination or a perceived lack of risk in contracting the virus in question are all cited as barriers to establishment of effective vaccination programmes for the elite athletic population [11] [12].
- Attitudes of elite athletes specifically with regards to the COVID-19 vaccine have yet to be elucidated.
- Following COVID vaccination, the elite athlete population have reported arm pain and fatigue as common side effects, the rates being more frequent after the second dose [13]
- More serious side effects such as myocarditis and thrombosis remain low, but not zero [14].
Conclusion
- Significant differences in COVID-19 screening and vaccination policy exist between the Tokyo 2020 and Beijing 2022 Olympic and Paralympic Games for athletes most notably in;
- extra precautions in the unvaccinated
- mask type
- close contact procedures
Authors and Affiliations:
Dr. Frank O’ Leary, Imperial College Healthcare NHS Trust francis.oleary1@nhs.net
Dr. Ajayi Abosede, Dept. Emergency Medicinem Imperial College Healthcare NHS Trust
Dr. Jonathan Korgaonkar, Dept. Sports & Exercise Medicine, Imperial College Healthcare NHS Trust
Competing interests: none
References:
[1] International Olympic Committee. Beijing 2022 Playbooks. [Internet]. 2021 [updated 2021 Dec 13; cited 2022 Jan 1st]. Available from: https://olympics.com/ioc/news/version-2-of-the-beijing-2022-playbooks-published.
[2] Tarrant M, Challis EB. Influenza vaccination for athletes? CMAJ. 1988;139:282.
[3] Gundlapalli AV, Rubin MA, Samore MH, Lopansri B, Lahey T, McGuire HL et al. Influenza, Winter Olympiad, 2002. Emerg Infect Dis. 2006;12:144-146.
[4] International Olympic Committee. Tokyo 2020 Playbooks. [Internet]. 2021 [updated 2021 Jun 15; cited 2022 Jan 1st]. Available from: https://olympics.com/ioc/tokyo-2020-playbooks.
[5] International Olympic Committee. New data shows no COVID-19 spread between Tokyo 2020 participants and local population. [Internet]. 2021 [updated 2021 Dec 31; cited 2022 Jan 1st]. Available from: https://olympics.com/ioc/news/new-data-shows-no-covid-19-spread-between-tokyo-2020-participants-and-local-population.
[6] Jaworski CA, Rygiel V. Acute Illness in the Athlete. Clinics in Sports Medicine. 2019; 38:577-595.
[7] Young M, Fricker P, Maughan R, MacAuley D (1998) The travelling athlete: issues relating to the Commonwealth Games, Malaysia. Br J Sports Med. 32:77–81.
[8] Collins CJ, O’Connell B (2012) Infectious disease outbreaks in competitive sports, 2005-2010. J Athl Train. 47:516–518.
[9] Thakur V, Kanta Ratho R. OMICRON (B.1.1.529): A new SARS-CoV-2 Variant of Concern mounting worldwide fear. J Med Virol [Internet]. 2021 Dec [cited 2022 Jan 1]; 2021 Dec 22. Available from: https://pubmed.ncbi.nlm.nih.gov/34936120/.
[10] Löllgen H, Bachl N, Papadopoulou T, et al. Infographic. Clinical recommendations for return to play during the COVID-19 pandemic. British Journal of Sports Medicine 2021;55:344-345.
[11] Signorelli C, Odone A, Miduri A et al. Flu vaccination in elite athletes: a survey among Serie A soccer teams. Acta Biomed. 2016;87:117–120.
[12] O’ Leary F, O’ Donovan J. Attitudes of elite athletes and their support staff to the influenza vaccine. Ir J Med Sci. 2021;190(3):1231-1236.
[13] Hull JH, Wootten M, Ranson C. Tolerability and impact of SARS-CoV-2 vaccination in elite athletes. Lancet Respir Med. 2022 Jan [cited 2022 Jan 3]; 10(1):e5-e6. Available from: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00548-8/fulltext.
[14] Patone, M., Mei, X.W., Handunnetthi, L. et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2021 Dec [cited 2022 Jan 3] Available from: https://doi.org/10.1038/s41591-021-01630-0.