The short answer is yes, you should!
Physical activity has a wide range of benefits for many different outcomes in almost all cancer cases. These include, but are not limited to, physiological outcomes like cardiopulmonary fitness, physical function and body composition, and patient-reported outcomes including fatigue, sleep, and sense of empowerment (Hojman, Gehl, Christensen, & Pedersen, 2018). At present, we do not fully comprehend all the complex mechanisms involved in the effect of exercise on cancer, but the effects seem to have a positive impact independent of age and gender (Hojman et al., 2018).
Benefits of physical activity in cancer survivors
A cancer tumor is part of some tissue in the body, meaning that whatever you expose your body to, you also expose the tumor to. This is an advantage if we choose to expose our body to cancer killing or cancer inhibiting substances or environments. When physically active, our bodies produce a lot of different substances that target the cancer cells, while the increased temperature and acute stress environment caused by physical activity make an unfavorable environment for the tumor (Hojman et al., 2018; Idorn & Hojman, 2016). This can further impact the rate of tumor growth and the risk of spreading, and the inhibitor effect of physical activity is evident across most investigated cancer types (Hojman et al., 2018). Physical activity can also strengthen the immune system, making it more efficient in inhibiting tumor growth and aiding treatment side effects and toxicity.
Regular exercise increases blood flow and formation of blood vessels throughout the body. When blood circulation and oxygen delivery to cells are improved, it can impact how well chemotherapy reaches the tumor and promote the effect of radiotherapy, while increasing overall tolerance of the medications (Esteves, Monteiro, & Duarte, 2021; Hojman et al., 2018).
In most cases of solid tumors, the primary treatment is surgery. Being physically active before surgery can increase the patients’ physical capacity, making the operation safer, decreasing the length of hospitalization and the risk of death (Hojman et al., 2018).
Cancer and cancer treatment can increase the risk of developing new cancers or other chronic diseases like cardiovascular disease, osteoporosis, and type 2 diabetes (Spence, Sandler, Newton, Galvão, & Hayes, 2020). Physical activity has proven to play an important role in the prevention and management of these conditions. Loss of muscle mass can occur as a result of the cancer itself, or because of the treatment. Gaining or retaining muscle mass before, during and after cancer treatment can have important implications for physical function, dependence on others, and various late effects.
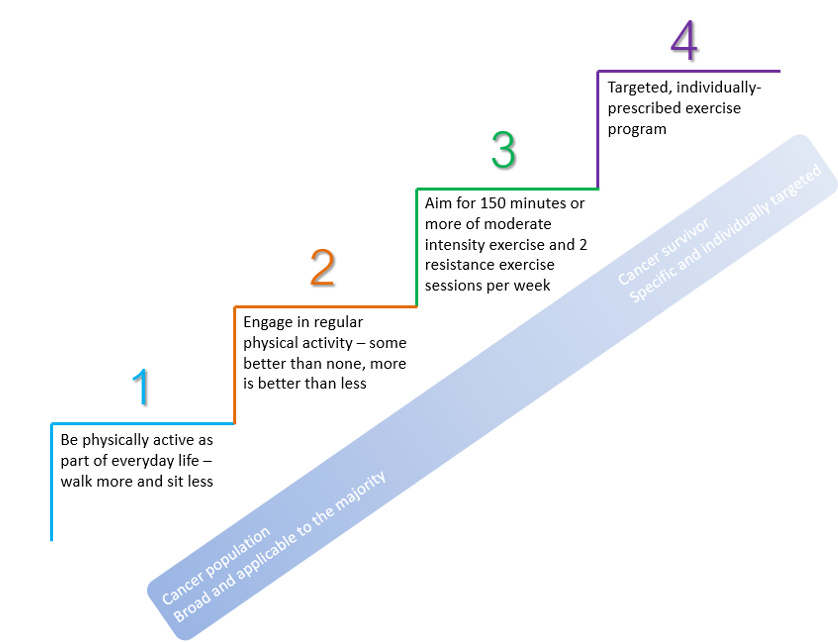
Recommendations
Cancer survivors are encouraged to engage in 150 minutes or more of at least moderate intensity (e.g., brisk walking) each week, and to include muscle strengthening exercises at least twice a week (Spence et al., 2020). A dose response relationship between physical activity and positive effects have been observed, where little is better than none, and more is better than little. Steep reductions in unfavourable outcomes are seen with amounts corresponding with the weekly recommended 150 minutes. Physical performance can even be increased during treatment, with very few (<5%), and no life threatening, adverse events (Bjørke et al., 2019; Spence et al., 2020).
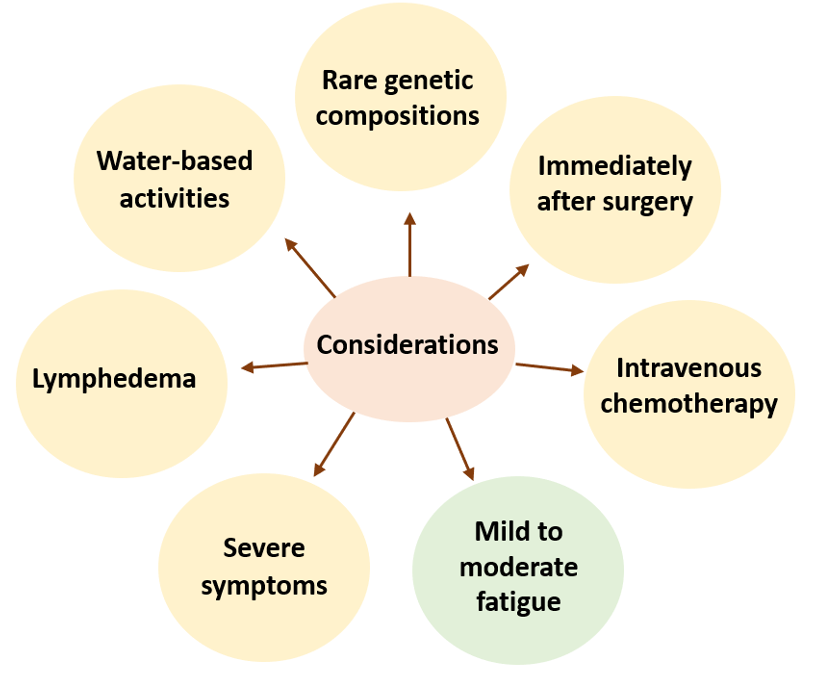
Some considerations
In a few rare cases, the genetic composition of the cancer make exercise less efficient in regulating the tumor (Hojman et al., 2018). Immediately after surgery, physical activity should be cleared by a physician, especially for movement of surgical wounds (Tucker, Staley, Clark, & Soper, 2019). Physical activity should not be performed at the day of intravenous chemotherapy and the consecutive 24 hours. Fitted compression garments can be used during activity in the case of lymphedema. Water-based activity can increase risks of infection in open wounds or when a catheter is used, or cause skin irritation after radiation therapy. In the case of extreme fatigue, severe anemia, current infection or fever, severe gastrointestinal symptoms and other severe musculoskeletal- or neurological symptoms, physical activity should be avoided for a period of time. In the case of mild to moderate fatigue, physical activity can help aid symptoms.
Increasing physical activity
For cancer survivors who lack experience with physical activity, participating in supervised group-based exercise sessions may be more feasible (Spence et al., 2020). Exercise should be individualized, taking into account overall health and physical function, motivation, and goals. For older and frail individuals, it may include some sit-to-stand exercises. For others it may include a 60-minute walk or playing squash. The most important thing is that it feels manageable and is something that can be maintained over time.
In other words, do not be afraid of trying out some activities even though you have been diagnosed with cancer. It can be good for both your mental and physical health, and support your body in fighting the cancer.
Author and Affiliations:
Benedikte Western is currently a PhD student at the Department of Sport Science and Physical Education, University of Agder, Norway.
References:
Bjørke, A. C. H., Sweegers, M. G., Buffart, L. M., Raastad, T., Nygren, P., & Berntsen, S. (2019). Which exercise prescriptions optimize V̇O2max during cancer treatment?—A systematic review and meta-analysis. Scandinavian journal of medicine & science in sports, 29(9), 1274-1287. doi:10.1111/sms.13442
Campbell, K. L., Winters-Stone, K. M., Wiskemann, J., May, A. M., Schwartz, A. L., Courneya, K. S., . . . Schmitz, K. H. (2019). Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Medicine and science in sports and exercise, 51(11), 2375-2390. doi:10.1249/mss.0000000000002116
Esteves, M., Monteiro, M. P., & Duarte, J. A. (2021). Role of Regular Physical Exercise in Tumor Vasculature: Favorable Modulator of Tumor Milieu. Int J Sports Med, 42(5), 389-406. doi:10.1055/a-1308-3476
Hojman, P., Gehl, J., Christensen, J. F., & Pedersen, B. K. (2018). Molecular Mechanisms Linking Exercise to Cancer Prevention and Treatment. Cell Metabolism, 27(1), 10-21. doi:https://doi.org/10.1016/j.cmet.2017.09.015
Idorn, M., & Hojman, P. (2016). Exercise-Dependent Regulation of NK Cells in Cancer Protection. Trends in Molecular Medicine, 22(7), 565-577. doi:https://doi.org/10.1016/j.molmed.2016.05.007
Spence, R. R., Sandler, C. X., Newton, R. U., Galvão, D. A., & Hayes, S. C. (2020). Physical Activity and Exercise Guidelines for People With Cancer: Why Are They Needed, Who Should Use Them, and When? Seminars in Oncology Nursing, 151075. doi:https://doi.org/10.1016/j.soncn.2020.151075
Tucker, K., Staley, S.-A., Clark, L. H., & Soper, J. T. (2019). Physical Activity: Impact on Survival in Gynecologic Cancer. Obstet Gynecol Surv, 74(11), 679-692. doi:10.1097/OGX.0000000000000731