In my previous blog I reviewed the excellent RESTORE study1, which concluded no benefit for platelet-rich plasma (PRP) over saline injection for knee osteoarthritis (OA) (according to the authors) and which no doubt will be used to justify exclusion of funding for PRP injections, despite previous reviews showing likely benefit2-6. Even though knee OA has very few evidence-based treatments, mainstream medicine groups don’t want to consider PRP as a treatment and RESTORE will be used (justifiably, to an extent, as the results were disappointing) to continue freezing out PRP from funding within medical systems7.
Don’t @ me, but PRP is better than cortisone
If you want any further evidence that there is a cultural war going on, look no further than the response of mainstream medicine to the McAlindon 2017 JAMA study8. This study showed far more dismal results for corticosteroid injections than the RESTORE study showed for PRP. There was no clinical benefit to corticosteroid (in fact unlike PRP it did worse than saline) and you also got significantly more cartilage degeneration to go with the lack of any clinical benefit. In response to McAlindon, we’ve heard “crickets” from medicine’s ruling class. Corticosteroid injections are still recommended by guidelines published subsequent to McAlindon9 10, still funded almost everywhere, and still by far the most common injection type. If you can’t afford to privately pay for exercise treatment, or PRP injections (both of which are not generously funded by health systems), you will get offered “free” corticosteroid injections under most medical systems. Even though the results for corticosteroid injections are clearly worse than PRP and exercise.
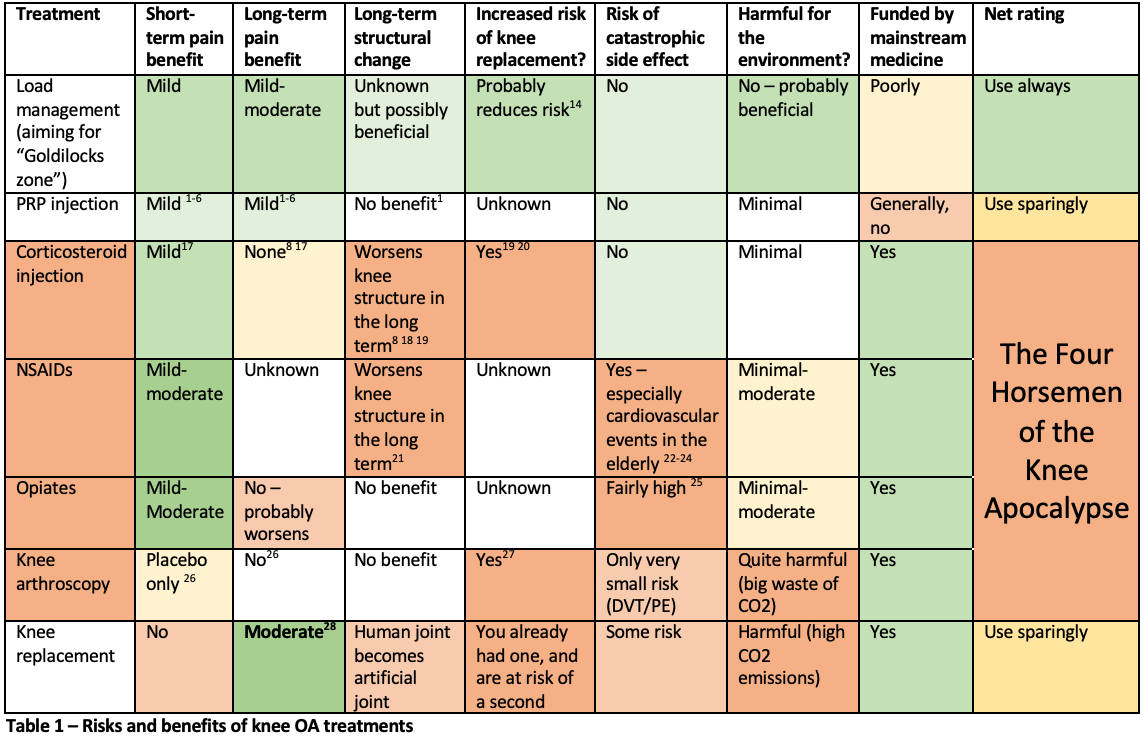
There are some 8 RCTs directly comparing PRP to corticosteroid and – surprise surprise – they favour PRP individually (e.g. 11 12) and when entered into a meta-analysis13. But culture war will ensure that – for a while yet – the darling treatments of mainstream medicine – knee arthroscopy, NSAIDs, opiates and corticosteroid injections (my “four horsemen of the knee apocalypse”, Table 1), will continue to get funded by most medical systems around the world.
The four horsemen of the knee apocalypse
The harmful four of knee arthroscopy, NSAIDs, opiates and corticosteroid injections all are harmful in slightly different ways, as I outline in Table 1. And I accept that individually there can be circumstances for each of the four where they are justified, but don’t accept that they are so commonly used in situations where risks outweigh the benefits. Yes Table 1 is not peer reviewed – but my response is that Table 1 is based on published studies. It might not pass peer review because of “culture wars”. Also, I don’t include all knee OA treatments in Table 1 – hyaluronan gel is another similar treatment to PRP with somewhat borderline status; almost certainly preferable to corticosteroid but not as good as load management.
So how can we rise above the culture war? Of course the best management of knee OA is exercise therapy or more specifically load management. It is very hard to adequately randomise exercise (over a long time period) in a randomised trial, but observations of populations show that those who exercise in the Goldilocks zone (not too much, not too little) get fewer knee osteoarthritis symptoms14 and also the general health benefits of exercise15.
Exercise therapy is the “solar panels” of musculoskeletal treatment
Adding exercise is the correct treatment for somebody who is not loading enough, but adding exercise is incorrect treatment for somebody who is loading too much (hence load management > exercise therapy). Load management is the electric vehicle or solar panel equivalent in the knee OA treatment armory and is inadequately funded so, sadly, entire populations don’t get great access to this treatment. Knee arthroscopy, NSAIDs, opiates and corticosteroid injections are the fossil fuel equivalents, all (net) harmful and all still funded heavily by the strong arm of vested interests, who promote mainstream medicine “always knows best” as part of a culture war. I see knee replacement as a potentially-valuable but highly-invasive treatment for end stage knee OA that you preferably don’t want to have (i.e. you don’t want your knee OA to get so bad that you need a replacement). I see PRP injections as being like a hybrid fossil fuel/electric vehicle. If you can get pain relief from PRP injections, it has very few of negatives of the nastier treatments and hence is better than them. But it is not as good as load management. Furthermore on the analogy with climate change mitigations, we need to try to reduce the carbon footprint of medical treatments themselves, particularly poor medical treatments.
Mainstream medicine has many, many great treatments, and we’d like the ruling views of mainstream medicine to be always in alignment with the scientific evidence. It has been very frustrating to have lived through a pandemic where a highly beneficial intervention (COVID vaccination) which is promoted appropriately by mainstream medicine is part of a culture war against an anti-vaxxer mob that has decided it doesn’t trust mainstream medicine. But it is equally frustrating to practice in musculoskeletal medicine where mainstream medicine is promoting/funding so many dubious knee OA treatments7 and is frankly refusing to switch to (the very few) better options. Table 1 is a sorry tale of inappropriate treatments getting promoted and funded which is the reason why our outcomes (on knee OA) in the Western World keep getting worse16.
Author and Affiliations:
John Orchard @DrJohnOrchard AM MD PhD FACSEP FFSEM (UK) FACSM
References:
- Bennell KL, Paterson KL, Metcalf BR, et al. Effect of Intra-articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis: The RESTORE Randomized Clinical Trial. Jama 2021;326(20):2021-30.
- Nie LY, Zhao K, Ruan J, et al. Effectiveness of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Clinical Trials. Orthopaedic journal of sports medicine 2021;9(3):2325967120973284.
- Laudy A, Bakker E, Rekers M, et al. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med 2015;49(10):657-72.
- Hohmann E, Tetsworth K, Glatt V. Is platelet-rich plasma effective for the treatment of knee osteoarthritis? A systematic review and meta-analysis of level 1 and 2 randomized controlled trials. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie 2020;30(6):955-67.
- Dai WL, Zhou AG, Zhang H, et al. Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Trials. Arthroscopy 2017;33(3):659-70.
- Hong M, Cheng C, Sun X, et al. Efficacy and Safety of Intra-Articular Platelet-Rich Plasma in Osteoarthritis Knee: A Systematic Review and Meta-Analysis. BioMed research international 2021;2021:2191926.
- Orchard J, Moen MH. Has reimbursement for knee osteoarthritis treatments now reached ‘postfact’ status? Br J Sports Med 2017;51(21):1510-11.
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. Jama 2017;317(19):1967-75.
- Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis & rheumatology (Hoboken, NJ) 2020;72(2):220-33.
- Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019;27(11):1578-89.
- Forogh B, Mianehsaz E, Shoaee S, et al. Effect of single injection of platelet-rich plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trial. J Sports Med Phys Fitness 2016;56(7-8):901-8.
- Elksniņš-Finogejevs A, Vidal L, Peredistijs A. Intra-articular platelet-rich plasma vs corticosteroids in the treatment of moderate knee osteoarthritis: a single-center prospective randomized controlled study with a 1-year follow up. Journal of orthopaedic surgery and research 2020;15(1):257.
- McLarnon M, Heron N. Intra-articular platelet-rich plasma injections versus intra-articular corticosteroid injections for symptomatic management of knee osteoarthritis: systematic review and meta-analysis. BMC Musculoskelet Disord 2021;22(1):550.
- Alentorn-Geli E, Samuelsson K, Musahl V, et al. The Association of Recreational and Competitive Running With Hip and Knee Osteoarthritis: A Systematic Review and Meta-analysis. J Orthop Sports Phys Ther 2017;47(6):373-90.
- Inge P, Perera N, Orchard J, et al. Exercise as Medicine—Evidence for Prescribing Exercise for the National Health Priority Areas: An Umbrella Review. J Postgrad Med Edu Res 2020;54(4):178-205, https://www.jpmer.com/abstractArticleContentBrowse/JPMER/22/54/4/22555/abstractArticle/Article.
- Singh JA, Yu S, Chen L, et al. Rates of Total Joint Replacement in the United States: Future Projections to 2020-2040 Using the National Inpatient Sample. J Rheumatol 2019;46(9):1134-40.
- Jüni P, Hari R, Rutjes A, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015:Oct 22;(10):CD005328.
- Pelletier JP, Raynauld JP, Abram F, et al. Intra-articular corticosteroid knee injection induces a reduction in meniscal thickness with no treatment effect on cartilage volume: a case-control study. Sci Rep 2020;10(1):13789.
- Zeng C, Lane NE, Hunter DJ, et al. Intra-articular corticosteroids and the risk of knee osteoarthritis progression: results from the Osteoarthritis Initiative. Osteoarthritis Cartilage 2019;27(6):855-62.
- Wijn SRW, Rovers MM, van Tienen TG, et al. Intra-articular corticosteroid injections increase the risk of requiring knee arthroplasty. The bone & joint journal 2020;102-b(5):586-92.
- Perry TA, Wang X, Nevitt M, et al. Association between current medication use and progression of radiographic knee osteoarthritis: data from the osteoarthritis initiative. Rheumatology (Oxford, England) 2021;60(10):4624-32.
- Barcella CA, Lamberts M, McGettigan P, et al. Differences in cardiovascular safety with non-steroidal anti-inflammatory drug therapy-A nationwide study in patients with osteoarthritis. Basic & clinical pharmacology & toxicology 2019;124(5):629-41.
- Schmidt M, Sørensen HT, Pedersen L. Diclofenac use and cardiovascular risks: series of nationwide cohort studies. Bmj 2018;362:k3426.
- Lu J, Wang L, Bennamoun M, et al. Machine learning risk prediction model for acute coronary syndrome and death from use of non-steroidal anti-inflammatory drugs in administrative data. Sci Rep 2021;11(1):18314.
- Morin KA, Vojtesek F, Acharya S, et al. Evidence of Increased Age and Sex Standardized Death Rates Among Individuals Who Accessed Opioid Agonist Treatment Before the Era of Synthetic Opioids in Ontario, Canada. Cureus 2021;13(10):e19051.
- Thorlund JB, Juhl CB, Roos EM, et al. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. Bmj 2015;350:h2747.
- Rongen JJ, Rovers MM, van Tienen TG, et al. Increased risk for knee replacement surgery after arthroscopic surgery for degenerative meniscal tears: a multi-center longitudinal observational study using data from the osteoarthritis initiative. Osteoarthritis Cartilage 2017;25(1):23-29.
- Skou ST, Roos EM, Laursen MB, et al. A Randomized, Controlled Trial of Total Knee Replacement. New England Journal of Medicine 2015;373(17):1597-606.