Person-centred experience for telerehabilitation following Anterior Cruciate Ligament Reconstruction – part of the Association of Chartered Physiotherapists in Sports and Exercise Medicine’s blog series
The rationale for this project is to co-design (1) alternative ways of engaging with patients using telehealth frameworks (2) and provide person-centred rehabilitation post-surgical reconstruction for anterior cruciate ligament injury (ACL-R).
Rationale for ‘Group’ Telerehabilitation Following Anterior Cruciate Ligament Reconstruction
Anterior Cruciate Ligament Reconstruction (ACL-R) surgery is a common procedure. (3) However, despite around 80% of ACL-R patients returning to some kind of sporting activities, only 65% return to their pre-injury level and 55% to competitive sport (4). Inadequate rehabilitation has been cited alongside poor preparation for return to sport as factors which could limit sporting performance and predispose to re-injury (5) (6) (7) . A systematic review with meta-analysis by Wiggins et al. (2016) estimated approximately 20% of those returning to sport following ACL-R experience a second ACL injury (8). With a heterogeneous selection of ACL-R rehabilitation protocols available online (9) and within the literature, (10) in conjunction with the disruption to physiotherapy rehabilitation services during the COVID-19 pandemic, it could be argued that a perfect storm has been created for poor provision for those rehabilitating from ACL-R. This could be exacerbated as orthopaedic services resume without the follow through capacity to adequately rehabilitate post-surgery.
Co-design of Novel Telerehabilitation Products and Processes Following ACL-R
Use of co-design in healthcare environments is relatively new (11) with no standard model for doing so being applied. Indeed, it is noted by Brocklehurst et al. (2018) that many different methodologies could be used (12) with co-design involving collaborative and evolving processes, with ownership and a practical focus being key according to some (13). With involvement of stakeholders to broaden the range of available ideas and gain their views being central in underpinning patient-centred rehabilitation (14) (15) post ACL-R, it was deemed prudent to harvest patients’ views in constructing the novel telerehabilitation products and processes. This was initially done via an on-line survey, link below:
On-line video resources with pertinent points of the rehabilitation exercises are currently being produced, as this was identified from survey results by patients as an important part of their ACL-R rehabilitation, particularly during the ongoing COVID-19 pandemic with a continuing reduced capacity for face-to-face physiotherapist engagement.
As this pilot for ‘Group’ telerehabilitation post ACL-R is rolled out, support for patients is provided via video conferencing using Near Me Video facilities within NHS settings. This allows appropriate regressions or progressions to be made for the patient within an evidence based post ACL-R protocol which both the physiotherapist and patient have access too. As part of the monitoring the Knee Injury and Osteoarthritis Outcome Score (KOOS) is known to have validity and reliability in measuring the functional status and quality of life for patients following ACL-R and is valid for research purpose with competitive athletes (16).
For those patients wanting to return to sport the Strategic Assessment of Risk and Risk Tolerance (StARRT) Framework established in 2016 (17) is a good starting point for making return to play decisions post ACL-R.
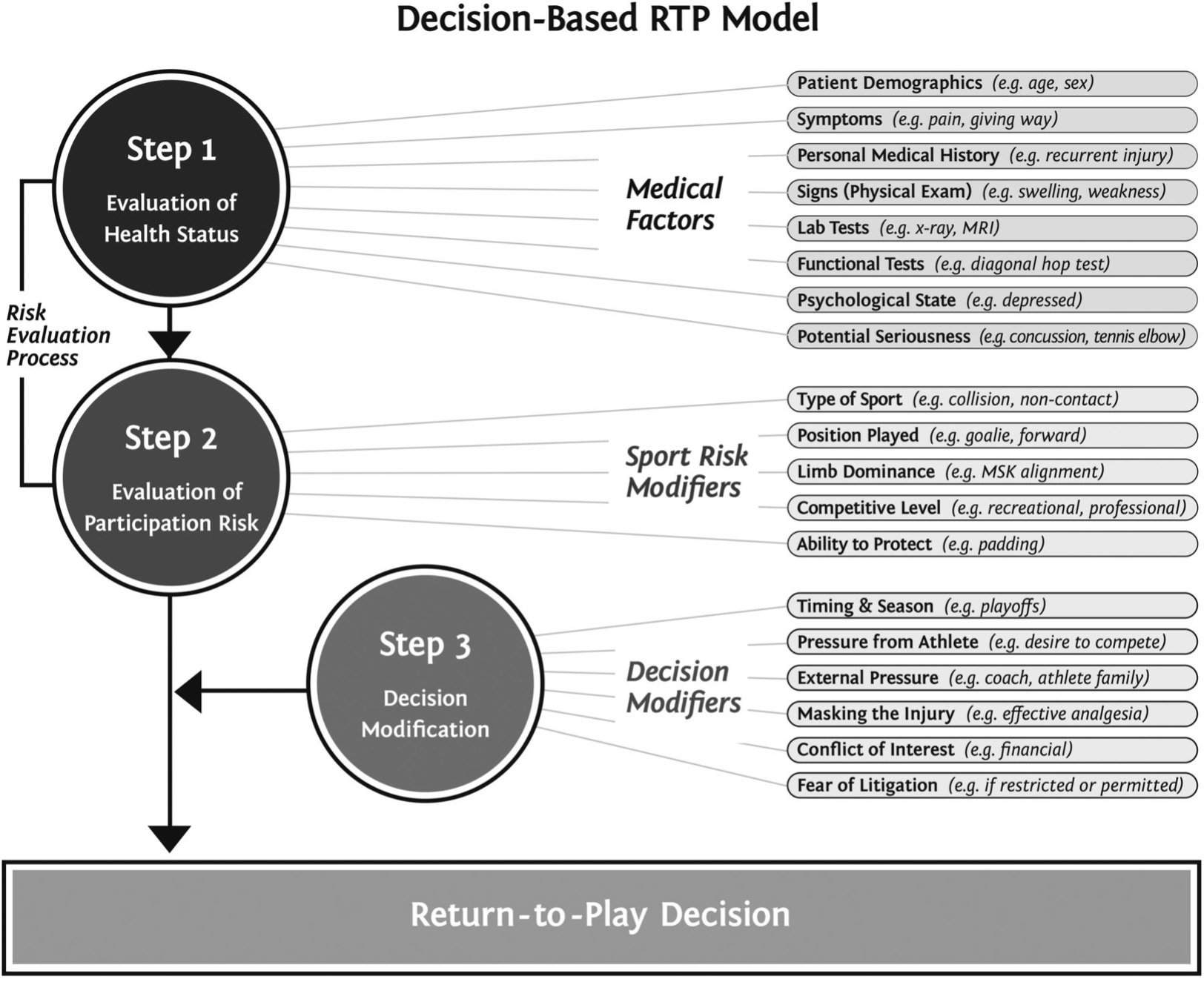
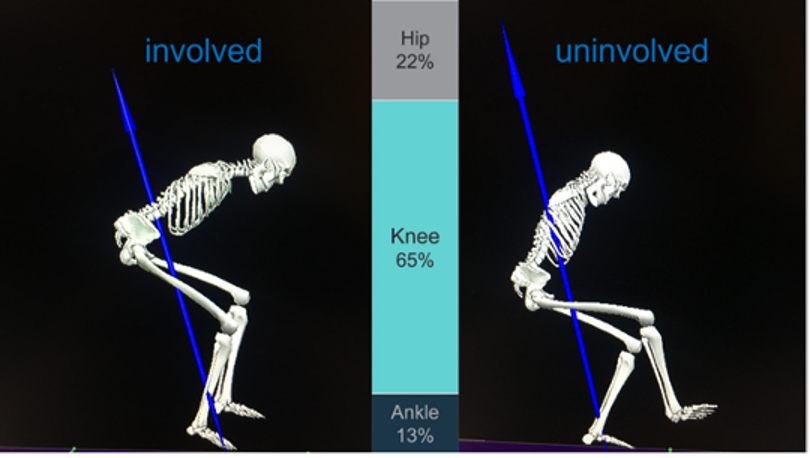
Return to play should be criteria based and be multi-disciplinary in nature (18) but exactly which criteria and how they should be used is controversial as discussed recently in BJSM Blog regarding the usefulness or otherwise of hop tests in ACL-R criteria (19).
Conclusions
- Telerehabilitation post ACL-R could address the difficulties associated with adequately preparing individuals for return to sport during the COVID-19 pandemic.
- Future work is needed to evaluate this pilot and further develop telerehabilitation products and processes based on participant co-design.
Authors and Affiliations: Jim Scanlan MSc; HCPC; CSP @jim_physio
NHS Fife Advanced Practitioner Physiotherapist Musculoskeletal & Orthopaedics
Association of Chartered Physiotherapists in Sports & Exercise Medicine: Silver Accreditation
Watsonians FC 1st XV Physiotherapist
Acknowledgements: Thank you to the Association Chartered Physiotherapists in Sports and Exercise Medicine @physiosinsport and British Journal of Sports Medicine @BJSM_BMJ for their support in publishing this Blog.
Competing Interests: Thank you to National Education for Scotland (NES) @NESnmahp for award of fellowship funding in order to undertake this project and for the support of NHS Fife @nhsfife

References:
- Batalden M, Batalden P, Margoalis P, et al. “Coproduction of Health Service”. British Medical Journal of Quality and Safety 2016;0:1-9
- Theodoros D, Hill A, Hartley N, et al. (2016) Innovation to Implementation for Telehealth: A Practical Guide to Knowledge Translation in Telehealth. CRE in Telehealth, Australia [online]. Viewed 14th May 2021. https://cretelehealth.centre.uq.au/files/501/I21-4-Telehealth-Nov2016.pdf
- Moses B, Orchard J, Orchard, J. Systematic review: annual incidence of ACL injury and surgery in various populations. Res Sports Med 2012;20:157-79
- Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014;48:1543–52
- Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 2016;50:804–8
- Kyritsis P, Bahr R, Landreau P, et al. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med 2016;50:946–51
- Ebert JR, Edwards P, Yi L, et al. Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26:2353–61
- Wiggins AJ, Grandhi RK, Schneider DK, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 2016;44:1861–76
- Makhni EC, Crump EK, Steinhaus ME, et al. Quality and variability of online available physical therapy protocols from academic orthopaedic surgery programs for anterior cruciate ligament reconstruction. Arthroscopy 2016;32:1612–21
- Thrush C, Porter TJ, Devitt BM. No evidence for the most appropriate postoperative rehabilitation protocol following anterior cruciate ligament reconstruction with concomitant articular cartilage lesions: a systematic review. Knee Surg Sports Traumatol Arthrosc 2018;26:1065–73
- Palmer VJ, Weavell H, Callander R, et al. The participatory zeitgeist: an explanatory theoretical model of change in an era of coproduction and codesign in healthcare improvement. BMJ Medical Humanities 2019;45(3):247-257
- Brocklehurst PR, Mckenna G, Schimmel M, et al. How do we incorporate patients views into design of healthcare services for older people: a discussion paper, BMC Oral Health 2018;18:61
- Pierri P, Tsianakas V, Robert G. Experience based co-design and healthcare improvement: realizing participatory design in the public sector. The Design Journal 2015;18(2):227–248
- Hawkins J, Madden K, Fletche A, et al. Development of a framework for the co-production and prototyping of public health interventions. BMC Public Heath 2017;17:689–700
- Thabrew H, Fleming T, Hetrick S, et al. Co-design of e-health interventions with children and young people. Frontiers in Psychiatry 2018; 9(481): 1–6
- Salavati M, Akhbari B, Mohammad F, et al. Knee injury and Osteoarthritis Outcome Score (KOOS); reliability and validity in competitive athletes after anterior cruciate ligament reconstruction. Osteoarthritis and cartilage 2011;19(4):406–410
- Ardern C, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med 2016;50:853-862
- van der Horts N, Backx FJG, Goedhart EA, et al. Return to play after hamstring injuries in football (soccer): a worldwide Delphi procedure regarding definition, medical criteria and decision-making. Br J Sports Med 2017;51:1583-1591
- Kotsifaki R, Whiteley R, van Rossom S, et al. Single leg hop for distance symmetry masks lower limb biomechanics: time to discuss hop distance as decision criterion for return to sport after ACL reconstruction. BJSM. 2020. https://blogs.bmj.com/bjsm/2021/05/27/hop-distance-the-elephant-in-the-room/ (accessed 09 Jun 2021)