An Australian Perspective
Medical servicing is a key component of high performance sport. This blog is directed to therapists and trainers working in a COVID-19 environment in Australia, however principles discussed are applicable for all sports science and sports medicine staff across the world.
Examples of COVID-19 entering the sporting environment with spread to athletes despite practitioners and athletes following best practice guidelines is a good reminder of the highly virulent nature of COVID-19 and that it is not “business as usual”. Therefore, inherent risks in the delivery of manual therapy services need to be carefully managed. If the therapist or athlete has been unwell (even if mild) with symptoms of COVID-19 (fever, cough, sore throat, shortness of breath) or potential symptoms not explained by another cause (fatigue, myalgia, loss of taste or smell, gastrointestinal symptoms) or had contact with a known or suspected case of COVID-19 in the past 14 days, they must not attend training or treatment until cleared to do so by a medical doctor.
Mandatory completion of the freely available Australian Government COVID-19 infection control training module is recommended for all staff involved in medical service provision prior to contact with athletes. At the Australian Institute of Sport we extended this recommendation to all athlete facing staff, (including coaches and support staff) to increase their health literacy, and leave staff well placed to guide athletes on hygiene practices.
In a sporting environment, treatment areas can often morph into an informal social gathering. Our approach to medical servicing is ‘get in, treat, get out’ to minimise number of individuals and unnecessary contact in treatment rooms and common areas in accordance with the social distance guidelines.
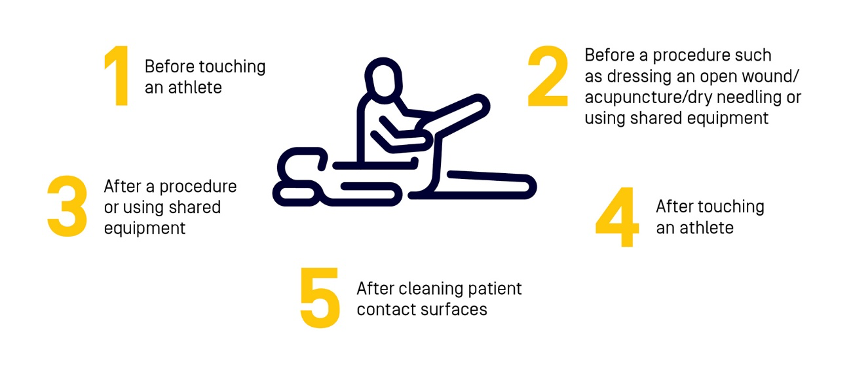
Hygiene is a key factor in transmission risk reduction and the Five moments of hand hygiene must be used. Re-usable bed linen has been removed and sharing of equipment is not advised. Thorough cleaning of treatment beds and key contact surfaces before and after every athlete is part of routine hygiene practice. Where available, the athlete and therapist wear a face mask during treatment sessions to reduce the risk of transmission in asymptomatic cases, as it is not possible to remain adequately distanced during manual therapy. Athletes are reminded to perform good hygiene practice at all times.
The AIS Framework divides sporting activity into three levels (A, B, C). Level A is the most restrictive level of training. Core principles for medical servicing specific to Level A, B, C sporting activities are discussed below.
Level A:
- All consultations should be conducted via telehealth where possible. Telehealth consults need to be conducted over end to end encrypted apps to ensure appropriate level of privacy is maintained.
- Consults should only proceed to face to face where considered essential and when all indirect management techniques have been exhausted, for example where the diagnosis cannot clearly be made without some differential physical assessment or where some equipment / technique is required to support athlete physical well-being.
- If face to face consults are essential public health advice on use of face masks should be followed and 1.5 m distancing should be maintained wherever practical.
- All routine and non-essential manual therapy should be avoided.
Level B:
- In line with the AIS Framework principles, all routine management consults should continue via telehealth where possible.
- Before considering face to face consults the therapist should consider whether they have exhausted all remote means of managing the athlete’s clinical presentation.
- Stakeholders must establish what the triggers are that support moving to the next level of servicing – for example, clinical improvement has plateaued and would benefit from an intervention from a therapist.
- Where possible, face-to-face consults should be conducted observing physical distance rules (i.e. from 1.5m apart) and hands on treatment should be for essential techniques only.
- A single source of therapist is recommended – it is recommended that sports and athletes seek to keep their manual therapists and sports trainers as part of their ‘bio security bubble’ to limit cross contact between sports and social groups.
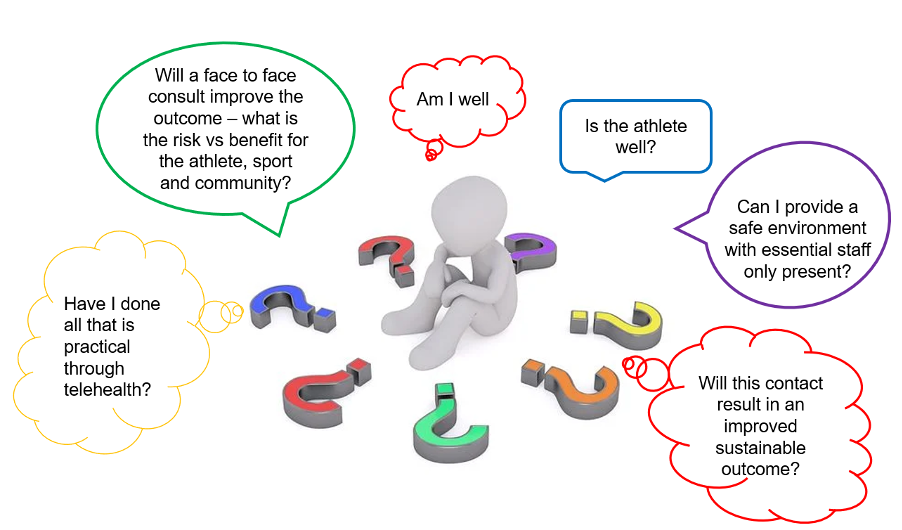
Considerations before arranging a face-to-face non-hands-on consult
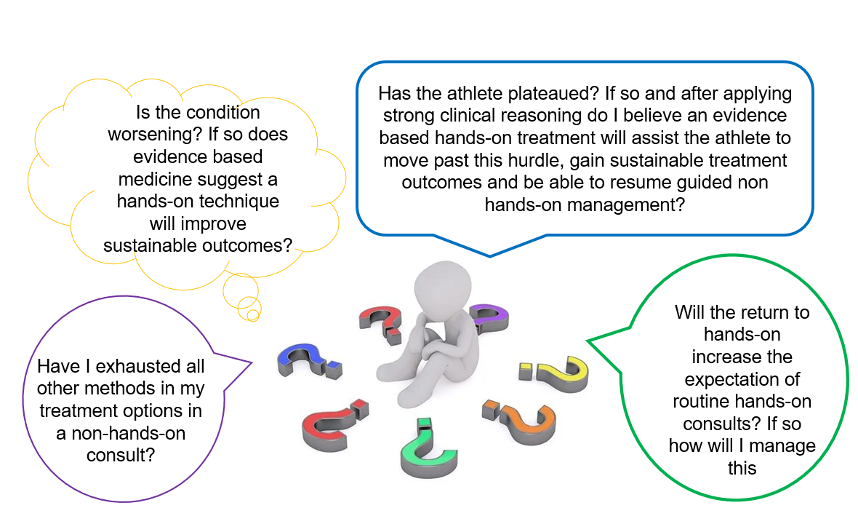
Considerations for follow up face-to-face hands-on consults
Level C:
- Physical distancing guidelines should be continued wherever practical.
- Where possible telehealth consults should continue to be considered as part of the assessment and management practices.
Planning and review of processes with a willingness and ability to implement change as required, along with strong support of public health messaging and practices will help keep sport a COVID-safe environment.
Authors & Affiliations:
Jennifer Cooke, Physiotherapy lead, Australian Institute of Sport
Nirmala Perera, Clinical Research Project Officer, Australian Institute of Sport
Richard Saw, Lead Physician, Australian Institute of Sport
David Hughes, Chef Medical Officer, Australian Institute of Sport