Building on last week’s podcast about biological healing with Professor Erik Witvrouw
Are injury recurrences due to a return to sport prior to adequate biological healing? Can we accurately measure stages healing with imaging or blood tests? On this BJSM podcast, Dr Liam West discusses the importance of respecting biological healing in musculoskeletal injuries with Professor Erik Witvrouw (Professor department of Rehabilitation Science and Physiotherapy at Ghent University). This podcast is packed to the rafters with top tips to rehabilitate injured athletes – let us know how you’ll be building them into your practice!
What do we think are some of the biggest lessons from this podcast?
It’s widely accepted that testing performance and quality of movement are key factors in determining when an athlete returns to play. However, determining the level that the athlete will return to, or how long they will stay free from injury that will be of real value to both player and coach alike.
Perhaps then it’s time we shifted our focus to assess how well an athlete has healed biologically?
Until now, prognostic indictors that included biological healing have been underutilised. Professor Witvrouw makes a strong case for respecting the biological healing process to strengthen the evidence base for when our athletes are ready to return to sport. This links well to Dubois and Esculier’s infographic that illustrates the complex rehabilitation of soft tissue injuries.
- 9 months is the earliest time MRI studies suggest ACL grafts in elite athletes are strong enough to allow return to sport – though it could be 2/3 years in total for grafts to mature fully.
- Muscular tears heal initially with immature scar tissue. 25% of reinjuries happen within the first week of return to play in the same location as the initial tear. This highlights the weakness of the immature scar tissue in the muscle/tendon itself.
- Elastography is a promising tool that can be used to assess ligamentous/tendon injuries. It may be particularly useful to assess patients with pathology in the same area as before. This is promising as it’s a first step to assessing when a patient is biologically ready to return to play, whereby a functional assessment could then follow.
- Inflammation leads to good healing. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) should be avoided in the early phase of injury – pain killers are fine, if required.
Want more resources on biological healing and return to play?
We are lucky within the BJSM community to have access to some world class research on relevant biological healing and return to play collections.
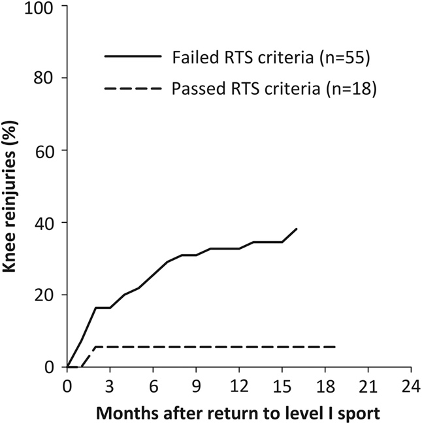
Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study #OpenAccess https://bjsm.bmj.com/content/50/13/804
For every month that return to sport was delayed, until 9 months after ACL reconstruction, the rate of knee reinjury was reduced by 51%.
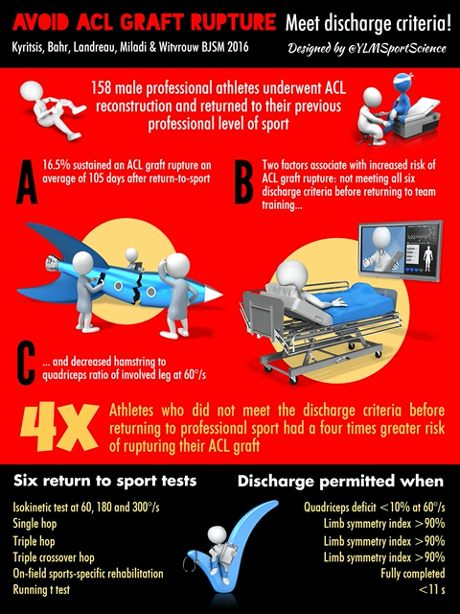
Infographic. Avoid ACL graft rupture. Meet discharge criteria https://bjsm.bmj.com/content/50/15/952
Why do discharge criteria exist? Turns out it’s for a reason! Athletes who did not meet the discharge criteria before returning to professional sport had a four times greater risk of sustaining an ACL graft rupture compared with those who met all six RTS criteria. In addition, hamstring to quadriceps strength ratio deficits were associated with an increased risk of an ACL graft rupture.
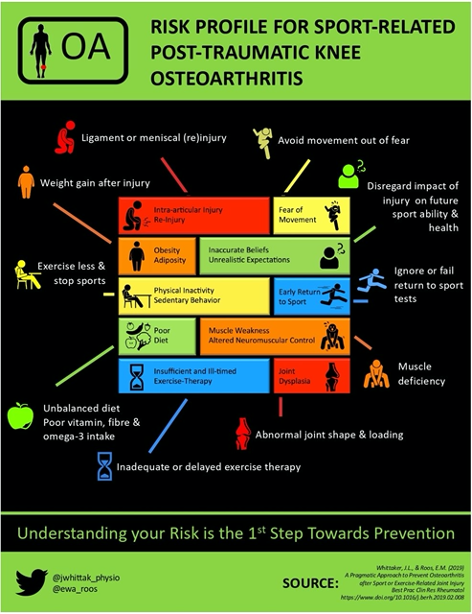
Infographic. Risk profile for sport-related post-traumatic knee osteoarthritis https://bjsm.bmj.com/content/54/6/362
To prevent osteoarthritis after a sport-related knee joint injury, we need to know who is at greatest risk for PTOA and how to intervene to mitigate this risk. This infographic outlines a risk profile for sport-related post-traumatic knee osteoarthritis with the aim of informing a pragmatic approach to prevention.The profile is based on what is currently known about modifiable factors that mediate the PTOA causal pathway or, increase the risk for or protect against knee PTOA itself. This includes established risk factors like intra-articular injury, elevated adiposity, physical inactivity, strength deficits or abnormal joint morphology.
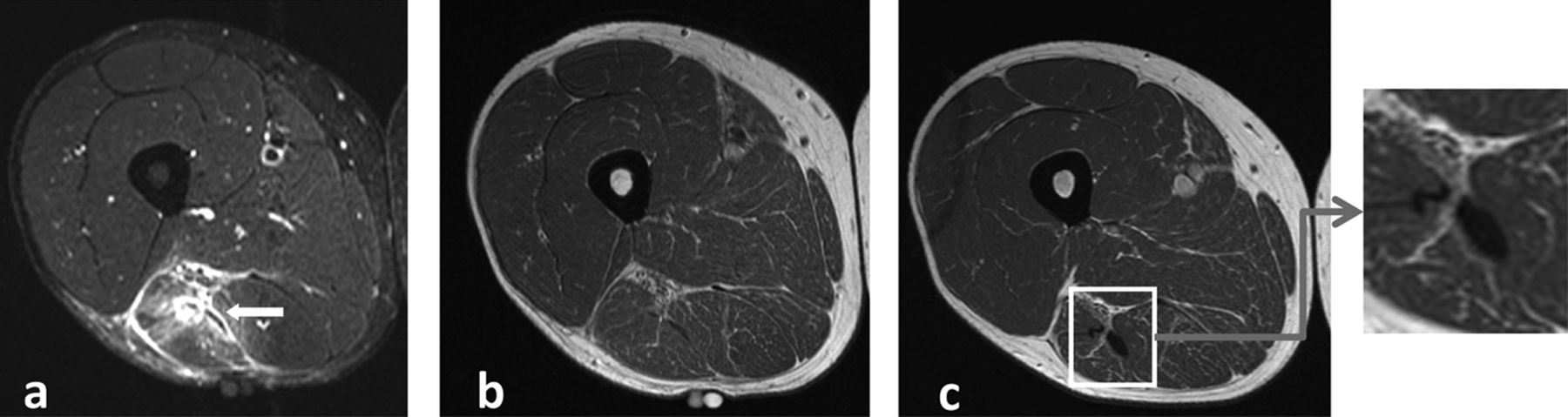
MRI observations at return to play of clinically recovered hamstring injuries #OpenAccess https://bjsm.bmj.com/content/48/18/1370
89% of clinically recovered hamstring injuries showed intramuscular increased signal intensity on fluid-sensitive sequences on MRI. Normalisation of this increased signal intensity seems not required for a successful RTP!
———
Blog by Jonny Elliott, Junior Doctor based in Belfast, Northern Ireland Representative Undergraduate Sports & Exercise Medicine Society (USEMS).