By Blaise Dubois @blaisedubois and Jean-Francois Esculier @JFEsculier
Rehabilitation of soft tissue injuries can be complex. Over the years, acronyms guiding their management have evolved from ICE to RICE[1], then to PRICE[2] and POLICE[3]. Although widely known, the evidence for these treatments is limited. ICE/RICE/PRICE focus on acute management and ignore sub-acute and chronic stages of tissue healing.
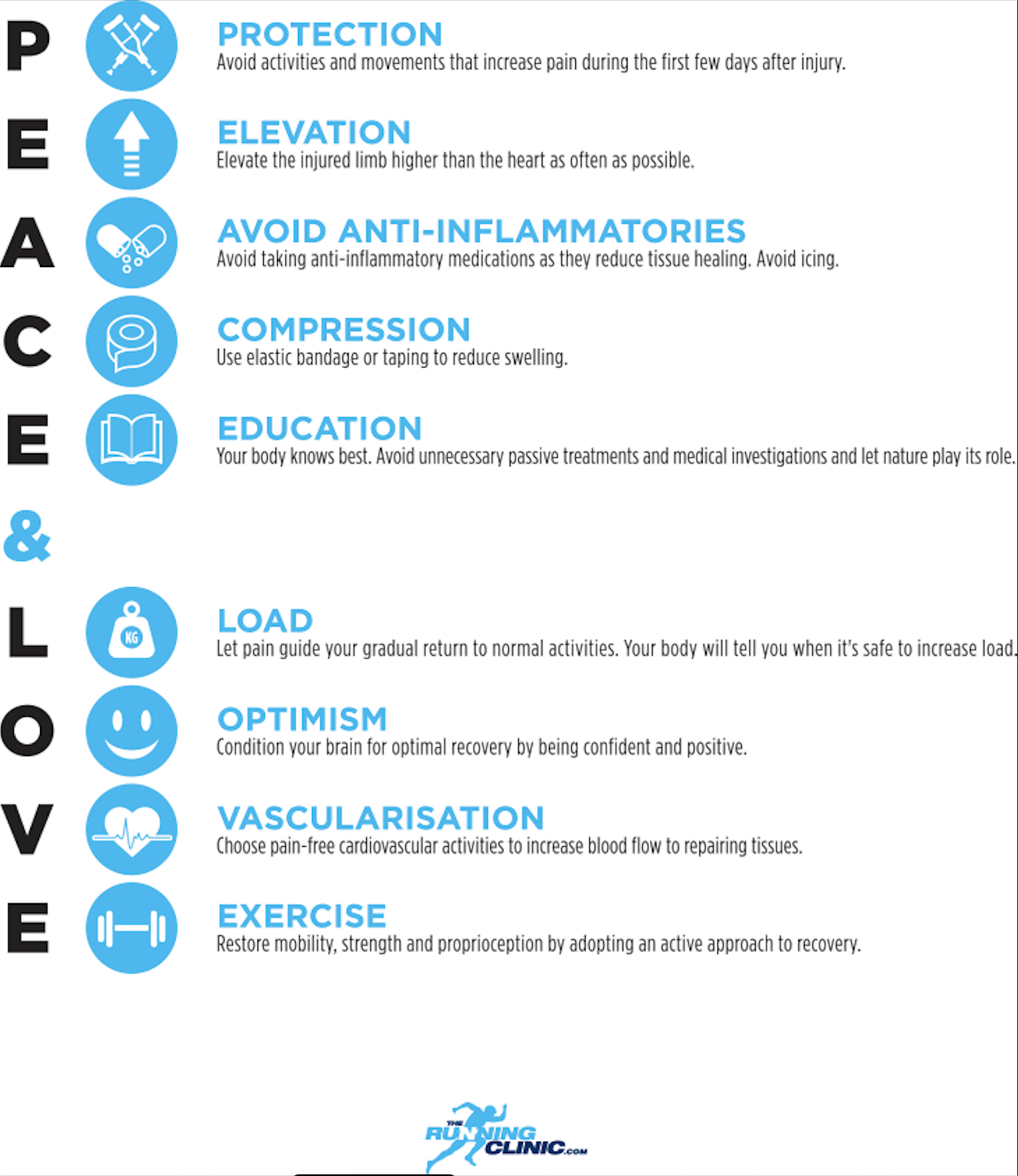
We posit that two new acronyms can optimize recovery. Our acronyms encompass the rehabilitation continuum from immediate care (PEACE) to subsequent management (LOVE). PEACE & LOVE underscores the importance of educating patients and addressing psychosocial factors to enhance recovery. In addition, while anti-inflammatories show benefits on pain and function, our acronyms flag their potentially harmful effects on optimal tissue repair.[4] We suggest that they may not be included in the standard management of soft tissue injuries.
Please see the full FREE paper in the BJSM here.
Do you agree with us? Let us know what you think! Tag us on Twitter with the hashtag #PeaceLove @blaisedubois @JFEsculier @BJSMPlus to continue the conversation.
PS- This blog and infographic are also available in French and Spanish!
***
Competing interests
None declared
Blaise Dubois (@blaisedubois) is the president and founder of The Running Clinic, an organization providing continuing education internationally. In the clinic and in research, Blaise is interested in the prevention and treatment of running injuries, with a particular focus on footwear and biomechanics. He is also an avid runner and co-owner of PCN physiotherapy clinics (Quebec City, Canada).
Jean-Francois Esculier (@JFEsculier) combines clinical research (Department of Physical Therapy, University of British Columbia) with patient care (Allan McGavin Sports Medicine Clinic, Vancouver) and knowledge translation (The Running Clinic, Canada). He loves to educate and empower patients so they can become the main actor of their rehabilitation. Email: jfesculier@therunningclinic.com
References
[1] van den Bekerom MPJ, Struijs PAA, Blankevoort L, et al. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults. J Athl Train2012;47: 435-43.
[2] Bleakley CM, Glasgow PD, Phillips N, et al. Guidelines on the management of acute soft tissue injury using protection rest ice compression and elevation. London: ACPSM, 2011.
[3] Bleakley CM, Glasgow P, MacAuley DC. Price needs updating, should we call the police? Br J Sports Med2012;46: 220-1.
[4] Vuurberg G, Hoorntje A, Wink LM, et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br J Sports Med2018;52: 956.
[5] Doherty C, Bleakley C, Delahunt E, et al. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br J Sports Med2017;51: 113-25.
[6] Duchesne E, Dufresne SS, Dumont NA. Impact of inflammation and anti-inflammatory modalities on skeletal muscle healing: From fundamental research to the clinic. Phys Ther Sport2017;97: 807-17.
[7] Yerhot P, Stensrud T, Wienkers B, et al. The efficacy of cryotherapy for improving functional outcomes following lateral ankle sprains. Ann Sports Med Res2015;2: 1015.
[8] Singh DP, Barani Lonbani Z, Woodruff MA, et al. Effects of topical icing on inflammation, angiogenesis, revascularization, and myofiber regeneration in skeletal muscle following contusion injury. Front Physiol2017;8: 93.
[9] Hansrani V, Khanbhai M, Bhandari S, et al. The role of compression in the management of soft tissue ankle injuries: A systematic review. Eur J Orthop Surg Traumatol2015;25: 987-95.
[10] Bleakley CM, O’Connor SR, Tully MA, et al. Effect of accelerated rehabilitation on function after ankle sprain: Randomised controlled trial. BMJ2010;340: c1964.
[11] Kim TH, Lee MS, Kim KH, et al. Acupuncture for treating acute ankle sprains in adults. Cochrane Database Syst Rev2014;6: CD009065.
[12] Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med2018;epub ahead of print, 25 June 2018.
[13] Graves JM, Fulton-Kehoe D, Jarvik JG, et al. Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health Serv Res2014;49: 645-65.
[14] Webster BS, Choi Y, Bauer AZ, et al. The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine2014;39: 1433-40.
[15] Khan KM, Scott A. Mechanotherapy: How physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med2009;43: 247-52.
[16] Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: Systematic review. Br J Sports Med2019;Epub ahead of print; 2019 Mar 2.
[17] Roy JS, Bouyer LJ, Langevin P, et al. Beyond the joint: The role of central nervous system reorganizations in chronic musculoskeletal disorders. J Orthop Sports Phys Ther2017;47: 817-21.
[18] Briet JP, Houwert RM, Hageman MGJS, et al. Factors associated with pain intensity and physical limitations after lateral ankle sprains. Injury2016;47: 2565-9.
[19] Bialosky JE, Bishop MD, Cleland JA. Individual expectation: An overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Phys Ther2010;90: 1345-55.
[20] Sculco AD, Paup DC, Fernhall B, et al. Effects of aerobic exercise on low back pain patients in treatment. Spine J2001;1: 95-101.