By Sarah Lindsay, Andy Massey, Robert Cooper, Sean Carmody, John Somauroo
Six months on from the first proposed case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and our world has been transformed. The World Health Organization (WHO) has categorised COVID-19 as a pandemic that is expected to pose a profound challenge on all aspects of life. Things will not return to normal for a long time and perhaps a ‘new normal’ will then exist as we learn to adapt and live with SARS-CoV-2. Global sporting events have been placed on hiatus during the pandemic, but we must keep in mind that sport has health, social and economic benefits for the individual and society.
Our challenge as physicians
As sports physicians it is our role to ensure athletes can complete fitness programmes and return to their sport whilst maintaining their safety. Some of these athletes have been infected with SARS-CoV-2 and some will become infected in the future. The challenge for us is to avoid complications from a virus which we are learning about in real time. There are many unknowns regarding the transmissibility of the virus, including asymptomatic carriage rate of SARS-CoV-21.
There have been reports of myocarditis in association with COVID-19, including cases in which myocarditis is proposed as the cause of death. Examination under autopsy showed infiltration of myocardium by interstitial mononuclear inflammatory cells2. Evidence of acute myocardial injury has been reported in up to 23% of patients hospitalised with COVID-193. Evidence of myopericarditis onset 1 week after initial mild COVID-19 related symptoms (isolated cough) has also been reported 4.
The incidence of arrhythmia in COVID-19 myocarditis is difficult to define, as most reports thus far have small sample sizes. In an early series reported from China 16.7% of patients hospitalised with COVID-19 had arrhythmias3, whilst arrhythmia was the reason for transfer to ITU in 44% of patients with COVID-195. It is feasible that arrhythmia could be related to direct myocyte injury, ischaemia from microvascular disease, pro-inflammatory cytokines and infection of the pericardium causing significant oedema.
Myocarditis has historically been proposed as the cause of SCD in up to 9% of cases6, therefore in the presence of active myocarditis, physicians advise patients to exercise less7. Whilst previous cases cannot have been due to SARS-CoV-2 specifically we must assume the disease process is similar. Reported myocarditis in those with COVID-19, combined with observations of arrhythmia in these patients, and previous observed risk of ventricular arrhythmia and SCD in myocarditis patients means we must be careful pushing athletes back to full activity following COVID-19 illness.
Athlete risk assessment
There are considerable economic and social incentives attached to resuming professional football. Should this occur prematurely it would present ethical and medical challenges. Robust risk assessment and mitigation procedures would facilitate professional football to return in some format despite the ongoing pandemic8, but they will not eliminate risk completely.
At the most fundamental level, cardiac assessment in athletes requires partnership with multiple members of the athlete care team. In elite sport we employ pre participation cardiac screening to identify athletes at risk of SCD. Universally, physicians recommend that the detection and management of cardiovascular diseases has the potential to reduce the incidence of SCD during athletic participation9,10.
The below model considers the evolving science pertinent to cardiac considerations for professional footballers following SARS-CoV-2 infection, with the overarching purpose to ensure the health and safety of players.
The Somauroo Model
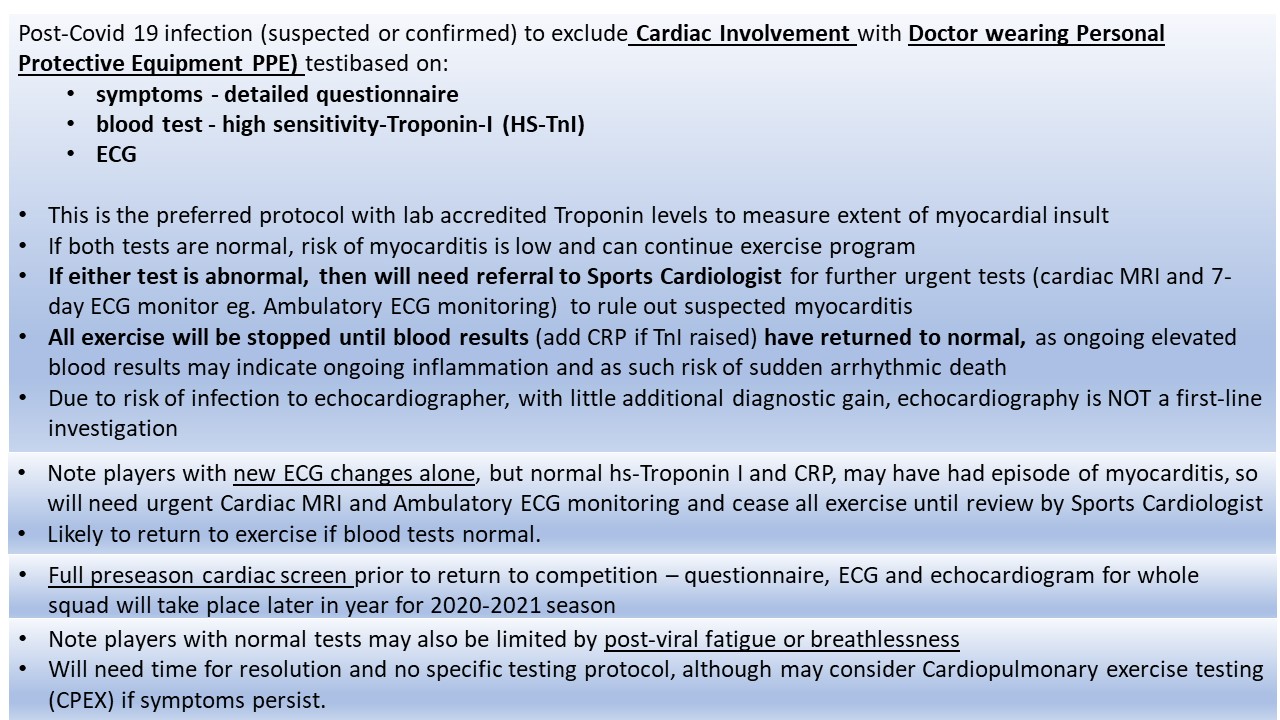
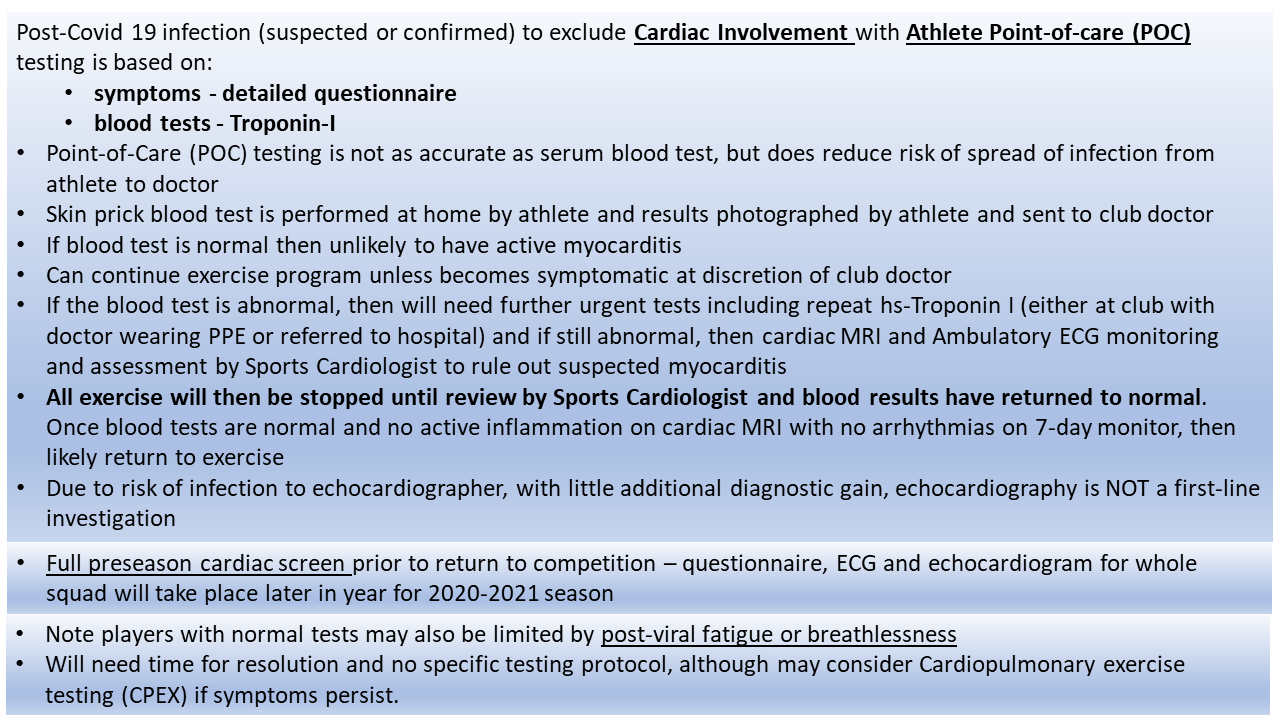
The possibility of myocarditis as part of the COVID-19 clinical syndrome needs to be considered prior to return to full training. We present The Somauroo Model (see PDF below, page 1) for return to professional sport post COVID-19, based on symptoms detailed by a questionnaire, ECG and blood tests (CRP and high-sensitivity Troponin). In our experience of this novel virus, if all 3 of these elements are normal, risk of myocarditis is low and the athlete can continue exercising. If any of the 3 are abnormal the athlete will need further urgent tests including cardiac MRI, ambulatory ECG monitoring and exercise test, with assessment by a Sports Cardiologist to rule out suspected myocarditis. The authors advise that all exercise be placed on hold until clearance to participate by a Sports Cardiologist is obtained and blood results have returned to normal (if elevated). Players with new significant ECG changes alone may have had an episode of resolved myocarditis. There is a high likelihood they will be able to return to exercise once significant pathology that increases the risk of SCD has been ruled out. Ongoing surveillance may be recommended for such athletes.
Given current restrictions in strained health services, risk of infection to echocardiographer, and little additional diagnostic gain in myocarditis, echocardiography has not been considered a first-line investigation. The protocol considers the restrictions that local or national governments may impose and is adapted accordingly to allow for tele-consults and self-testing by an athlete (if face-to-face contact is not possible due to the athlete’s location and risk of infection transmission) (see PDF below, page 2).
PDF with Samauroo Model (page 1) and Athlete Point-of-care Testing (page 2).
Summary:
***
Sarah Lindsay1,2, Andy Massey3, Robert Cooper4, Sean Carmody5, John Somauroo6
- Southport and Formby CCG, England
- Liverpool Football and Athletic Club, England
- Fédération Internationale de Football Association (FIFA), Zurich, Switzerland
- Institute of Cardiovascular Medicine and Science, Cardiology Department, Liverpool Heart and Chest Hospital, England
- Medical Department, Queens Park Rangers Football and Athletic Club, England
- Research Institute for Sport and Exercise Sciences, Liverpool John Moores University, Liverpool, UK
References
- Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Rivett L, Sridhar S, Sparkes D, et al. 2020 May 11;9.
- Xu Z, Shi L, Wang Y et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020;8: 420–22
- Gou T, Fan Y, Chen M et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiology 2020 27th March.
- Inciardi R et al. Cardiac Involvement In a Patient With Coronavirus Disease 2019. JAMA Cardiology. 2020 Mar 27
- Wang D, Hu B, Hu C, et al.: Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA – Journal of the American Medical Association American Medical Association, 2020; 323:1061–1069
- Harmon KG, Asif IM, Maleszewski JJ et al. Incidence, Cause, and Comparative Frequency of Sudden Cardiac Death in National Collegiate Athletic Association Athletes: A Decade in Review. 2015 Jul 7;132(1):10-9
- Pelliccia A, Solberg EE, Papadakis M et al. Eur Heart J. 2019 Jan 1;40(1):19-33. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC).
- UK Government, Coronavirus (COVID-19): what you need to do. https://www.gov.uk/coronavirus [Accessed 14th April 2020]
- Maron BJ, Thompson PD, Puffer JC, et al. Cardiovascular preparticipation screening of competitive athletes: a statement for health professionals from the Sudden Death Committee (clinical cardiology) and Congenital Cardiac Defects Committee (cardiovascular disease in the young), American Heart Association. Circulation 1996;94:850–6.
- Pelliccia A, Fagard R, Bjørnstad HH, et al. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J 2005;26: 1422–45.