By Robert-Jan de Vos @rj_devos and Edwin Oei

Patellar tendinopathy is an overuse injury that causes pain and impaired performance in jumping athletes. Prevalence is high in elite volleyball (45%) and basketball (32%) athletes.1 Symptoms can become long-standing Furthermore, there is currently no convincing evidence for second-line treatments such as shockwave therapy and platelet-rich plasma.2,3 Exercise therapy and load management are the best initial treatment options for tendinopathies. Therefore, it is important to improve exercise protocols as a first treatment of choice.
Does the type of exercise therapy really matter?
This is a question that a physiotherapist or sports physician can encounter when dealing with patients suffering from patellar tendinopathy. Exercise protocols can differ widely in design and hypothetical working mechanisms. The two extremes of protocols are (i) the progressive tendon-loading protocols with symptom-based progression criteria and (ii) the painful heavy-load eccentric exercises. There is currently no high-quality evidence to suggest one protocol above the other.
What is the background of the painful eccentric and the progressive tendon-loading exercise protocols?
Although painful eccentric exercise protocols have been promoted as standard care based on positive results in early studies4, a recent systematic review demonstrated that these are not associated with improved tendon structure and are ineffective when applied in-season.5 Progressive tendon-loading exercise therapy for patellar tendinopathy is a novel concept in sports medicine. A recent study advocated for a progressive 4-stage criteria-based exercise protocol with the aim of encouraging a less ‘reactive tendon’ and restoring collagen alignment.6 This protocol consisted of progressive isometric, isotonic, plyometric, and sport-specific exercises. Isometric exercises reduce pain and decrease motor cortex inhibition of the quadriceps muscle. This novel approach would enable jumping athletes to resume sports within the limits of pain, with improved muscle function, and possibly a sufficient tendon structure reorganisation.
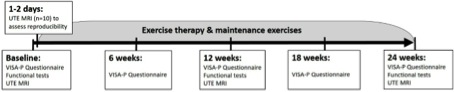
The primary aim of our research program that has recently been funded by GE Healthcare and the US National Basketball Association (NBA) is to assess whether the recently advocated 4-stage exercise protocol6 focusing on progressively developing load tolerance of the tendon (gradual adjustment) is more effective than the painful heavy-load eccentric exercise protocol7 (‘no pain, no gain’) for the treatment of patellar tendinopathy in jumping athletes. The secondary aim is to validate the novel 3D ultrashort echo time (UTE) MRI technique for quantitative imaging of the patellar tendon, by determining its responsiveness to exercise treatment, its correlation with clinical symptoms over time, and its predictive value of treatment response.
What is the novelty of the 3D Ultrashort echo time (UTE)-MRI technique?
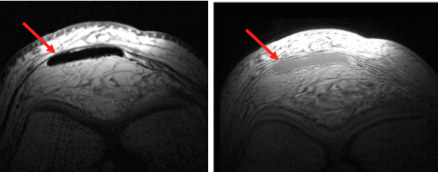
UTE-MRI is an innovative development in the field of tendon imaging.8 Unlike regular MRI techniques on which tendon structure typically is difficult to assess owing to the tendon’s low water content and resulting “black” appearance, UTE-MRI detects signal from tendons and visualises tendon abnormalities more accurately (Figure 1). Hence, with UTE-MRI it is possible to evaluate tendon structure and measure the amount of water in the tendon, both of which can be altered in tendinopathy, and which may improve after exercise therapy. While most research with UTE-MRI has been conducted with two-dimensional approaches based on a limited number of cross-sections acquired in the tendon, we will use a novel three-dimensional (3D) UTE-MRI method, provided to us as a research prototype from GE Healthcare. This software, which is not yet commercially available allows rapid imaging of the entire patellar tendon.
With current regular imaging modalities there is a disconnection between pathology on imaging and patient-reported pain. Identifying prognostic factors could lead to personalised medicine. Therefore, we additionally aim to develop novel quantitative 3D UTE MR imaging biomarkers for the assessment of patellar tendinopathy with the use of advanced image analysis and machine learning methods applied on the acquired MRI data.
What is the study design?
We will perform an open randomised controlled clinical trial. Jumping athletes aged 18-35 years will be studied. We aim to recruit basketball players and volleyball players who play at least three times per week and who have been diagnosed with patellar tendinopathy by a sports physician. The diagnosis of patellar tendinopathy will be made clinically with subsequent ultrasonographic confirmation to ensure that we will include patients with symptomatic patellar tendinopathy.
A total of 76 eligible patients will be randomly assigned to one of two different exercise protocols:
1) A progressive 4-stage criteria-based exercise protocol6
2) A 12-week painful heavy-load eccentric exercise protocol with subsequent maintenance exercises7
In both study groups, we will advise a standardised symptom-based return to sport during this period. Pain scores will be used to progress through the subsequent phases of return to sport in all athletes by a sports physician who is not involved in data acquisition. The time frame and outcome measures are displayed in Figure 2.
We will start the project in this summer and we expect to publish the results within 3 years after initiation.
References
- Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med 2005;33(4):561-7.
- Moraes VY, Lenza M, Tamaoki MJ, et al. Platelet-rich therapies for musculoskeletal soft tissue injuries. The Cochrane database of systematic reviews 2014;4:CD010071.
- Ioppolo F, Rompe JD, Furia JP, et al. Clinical application of shock wave therapy (SWT) in musculoskeletal disorders. Eur J Phys Rehabil Med 2014;50(2):217-30.
- Murtaugh B, Ihm JM. Eccentric training for the treatment of tendinopathies. Curr Sports Med Rep 2013;12(3):175-82.
- Drew BT, Smith TO, Littlewood C, et al. Do structural changes (eg, collagen/matrix) explain the response to therapeutic exercises in tendinopathy: a systematic review. Br J Sports Med 2014;48(12):966-72.
- Malliaras P, Cook J, Purdam C, et al. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J Orthop Sports Phys Ther 2015:1-33.
- Purdam CR, Jonsson P, Alfredson H, et al. A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. Br J Sports Med 2004;38(4):395-7.
- Juras V, Apprich S, Szomolanyi P, et al. Bi-exponential T2 analysis of healthy and diseased Achilles tendons: an in vivo preliminary magnetic resonance study and correlation with clinical score. Eur Radiol 2013;23(10):2814-22.
About the authors
Robert-Jan de Vos is a sports physician and post-doc researcher at the department of Orthopaedics in the Erasmus MC University Medical Centre in Rotterdam, the Netherlands. His research focuses on imaging and treatment of tendinopathies and injury prevention in football and running. He is also club doctor of Excelsior Football club.
Follow @rj_devos
Edwin Oei is a musculoskeletal radiologist and assistant professor at Erasmus MC University Medical Centre in Rotterdam, the Netherlands. His research focuses on advanced MRI techniques to study musculoskeletal disorders.