Undergraduate perspective on Sports & Exercise Medicine – a BJSM blog series
By Ted Caplan

With BASEM’s Spring Conference less than a week away, it is an apt time to reflect on the 2nd BASEM/FSEM Annual Conference in Cardiff (12th-13th November, 2015). This two-day event offered an in-depth look into: The Disabled Athlete, The Older Athlete, The Adolescent Athlete, Exercise in Health and Contact Sports. The programme also had sessions by the Society of Sports Therapists, FSEM, USEMS, ECOSEP and UKADIS.
The conference provided an excellent opportunity to hear from some of the leaders in the field of Sports and Exercise Medicine (SEM)- what follows are a few highlights.
Athletes with Disabilities Session
Boosting in Paralympic Sport – Protecting the Clean Athlete: Challenges for Education, Policy and Procedures (Prof Nick Webborn)
- Boosting is the intentional induction of autonomic dysreflexia (AD) in individuals with spinal cord injuries (T6 or above) to enhance athletic performance via greater release of catecholamines, larger V02 max’s and higher peak power (1)
- International Paralympic Committee (IPC) forbids athletes to compete in an AD state due to potential adverse consequences (e.g. cerebral haemorrhage, myocardial infarction and seizures). Interestingly, no reported performance-related AD adverse events.
- IPC Targeting testing in sports where boosting is possible, and in athletes who can become dysreflexic
- 7% of male athletes admitted to using AD to enhance performance (2), however no athletes found in a dysreflexic state in 7 year IPC screening programme. Perhaps screening protocols are not effective enough?
Activating Paralyzed Muscles: Necessary for Optimal Health? (Christof Smit MD)
- Muscle paralysis only tip of the iceberg for spinal cord injuries (SCI); multiple complications (e.g. spasticity, incontinence, respiratory problems, blood pressure issues etc)
- Arm exercises are unable to achieve sufficient intensity/durations and only activate small muscle masses
- Functional electrical stimulation (FES) improves muscle size/performance and enhances circulation
- FES activation of paralyzed muscles benefits individuals, attenuating several problems including pressure ulcers and low cardiovascular fitness
- FES enables individuals to raise daily energy expenditure, necessary to reduce the high prevalence of obesity in SCI. Ideally should be incorporated into the daily lives of all individuals with SCI
The Role of Upper Body Physical Activity in the Prevention of Metabolic Disease in Spinal Cord Injured Humans (Dr James Bilzon)
- Physical activity (PA) intervention can promote function and independence, whilst reducing biomarkers of cardiovascular and metabolic disease
- Adults with spinal cord injury (SCI):
- 4x as likely to develop Type 2 Diabetes (3)
- 2x more likely to suffer from Cardiovascular Disease (4)
- SCI individuals have reduced energy expenditure in comparison to able-bodied adults in multiple exercise/sport activities (e.g. weight training and table tennis) (5)
- Future research should determine exercise regimes that facilitate adherence and participation
Undergraduate Sports and Exercise Medicine Society (USEMS) Session
A Birds Eye View of SEM (Dr Rhodri Martin)
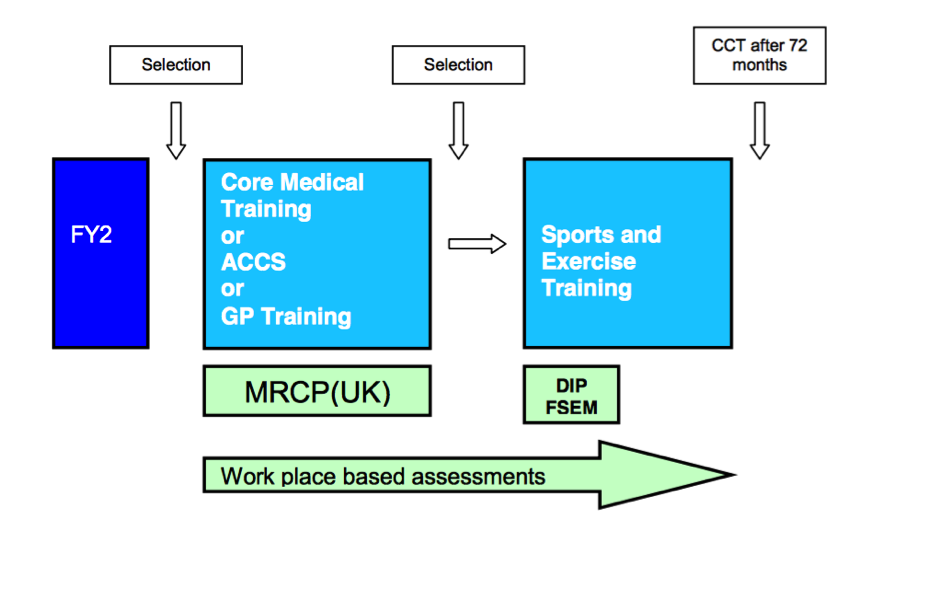
- In England, currently 41 trainees nationwide; Wales training programme is ‘on hold’. The current training pathway for SEM in the NHS is illustrated below:
- Currently, consultant level SEM physicians working for the NHS, Ministry of Defence, Institutes of Sport, Private Clinics, Professional Sport Teams and in Research
- Top Tips for Undergraduates
- Get involved at any level of sport (contact sport, trauma courses etc)
- Become involved in physical activity promotion
- Complete SSC/Research/Audits with relevance (ortho/rheum/cardio etc)
Movement is Medicine: The Bigger Picture – Movement as Medicine (Ms Ann Gates, @exerciseworks)
- “Movement is medicine: for patients, for the public, and for nations”
- Being aware of the big picture will enhance potential influence and leadership
- Inequalities still exist in our communities in terms of access
- Access to green spaces can increase physical activity for all ages, reduce health inequalities, increase levels of communal activity across different social groups and encourage active transport and community participation.
- Work needs to be conducted with education systems and schools, to make physical activity part of the curriculum. Children can greatly benefit from school and community policy changes.
Staring into the Crystal Ball of SEM (Dr Rod Jaques)
Dr Jaques spoke about the future of SEM from personal experiences and reflected on the following:
- The requirements of the SEM physician are ever-changing – learn to deal with uncertainty and adapt. “Be a chameleon”
- SEM challenges for the future:
- Look after your patients, not the sport
- Learn to sell yourselves and your services
- Inward-facing changes ahead – SEM curriculum, lack of jobs and training?
- Outward facing challenges – wellness has been construed as an individual’s own responsibility (i.e. not the government’s); less need for SEM specialty?
- Did the London 2012 Olympics help SEM? One positive outcome is that it has led to SEM specialty recognition
Imaging Muscle Injuries – A Clear Picture (Dr Steve James)
- Grading systems for injury determine the extent and severity of muscular injury, provide the clinician with prognostic information and guide therapeutic intervention (if required)
- British Athletics has introduced a new muscle injury grading system (see http://bjsm.bmj.com/content/48/18/1347)
- Poor prognostic factors for muscular injury on MRI:
- Higher cross-sectional area involvement
- Longer cranio-caudal length of injury
- Intratendinous involvement of injury
- Dr James’ approach to identifying and grading muscle injuries:
- Where is the injury? – Use axial fat suppressed/stir then axial T1
- Longitudinal extent of injury? – Use coronal/sagittal fat suppressed/stir
- Tendon rupture/ laxity? – Use coronal/sagittal T1
Top-, in Ten Minutes (Dr Bryn Savill)
- Make Your Own Way – What are your goals? Tailor your time to your goals.
- Be Unique – How can you stand out? Highlight your strengths
- Find the Balance – Enjoy what you do; however, think about the here and now; make sure you pass all of your exams
- Absorb SEM – Undertake a wide variety of experiences, the more the better. Immerse yourself
- Find a Mentor and Make Contacts – The best way to do this is to Network. Network. Network
References
- Schmid A, Schmidt-Trucksäss A, Huonker M, König D, Eisenbarth I, Sauerwein H, Brunner C, Storch MJ, Lehmann M, Keul J. Catecholamines response of high performance wheelchair athletes at rest and during exercise with autonomic dysreflexia. International journal of sports medicine. 2001;22(1):2-7
- Bhambhani Y, Mactavish J, Warren S, Thompson WR, Webborn A, Bressan E, De Mello MT, Tweedy S, Malone L, Frojd K, Van De Vliet P, Vanlandewijck Y. Boosting in athletes with high-level spinal cord injury: knowledge, incidence and attitudes of athletes in paralympic sport. Disability and rehabilitation. 2010;32(26):2172-2190.
- Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43(6):749-756.
- Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, Brown R. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. 2005;43(7):408-416
- Collins EG1, Gater D, Kiratli J, Butler J, Hanson K, Langbein WE. Energy cost of physical activities in persons with spinal cord injury. Medicine & Science in Sports & Exercise. 2010;42(4):691-700
Ted Caplan BSc (Hons) Sport Science in Relation to Medicine is a 4th year medical student at the University of Bristol, UK.
Dr. Liam West BSc (Hons) MBBCh PG Dip SEM is originally from the UK and now is a Resident Medical Officer in Melbourne, Australia. He coordinates the “Undergraduate Perspective on Sports & Exercise Medicine” Blog Series for BJSM.
If you would like to contribute to the Undergraduate Perspective on SEM BJSM Blog, please contact Dr. West at liamwestsem@hotmail.co.uk