Why we should consider neural structures around the distal musculotendinous junction of the biceps femoris
Keywords – Hamstring, Neural, Rehabilitation

Introduction – Hamstring injuries are the greatest cause of time loss within a wide range of elite sports, with injuries at the distal musculotendinous junction of the biceps femoris amongst the most problematic [1]. This blog will look to propose a theory as to why this may be.
The T–junction : Incidence, anatomy & mechanism of injury
The distal musculotendinous junction (T junction) of the biceps femoris is acknowledged as a problematic area for clinicians, with the most severe hamstring injuries in rugby union presenting in this region [2]. These specific injuries have been reported as having a recurrence rate of 54% which is considerably higher than general hamstring reinjury rates reported elsewhere in the literature [3]. These findings are also supported in a football cohort, with 56% of hamstring reinjuries occurring following injury in the distal third of the biceps femoris [4].
The reason behind this increased risk of re-injury has been proposed to be related to the complex and variable anatomy of the region (Figure 1). Of particular interest though is the dual innervation of the biceps femoris, with the long head innervated by the sciatic nerve and the short head by the common peroneal nerve.
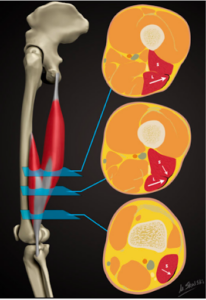
Figure 1 – Anatomy of the T-junction (Taken from Entwisle et al., 2017)
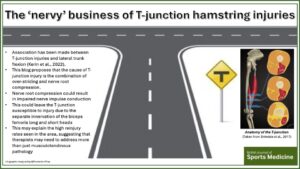
A study by Kerin et al (2022) suggested that 50% of hamstring injuries sustained within rugby union involved ipsilateral trunk flexion, with one specific case in the study linked to the T junction (See Figure 2). A previous British Journal of Sports Medicine blog has also anecdotally linked ipsilateral trunk rotation to T-junction injuries [6]. If this is the case and a mechanism of ipsilateral trunk flexion and rotation is likely linked to distal musculotendinous junction injuries, then it is important to understand why.

Figure 2- Mechanism of T-junction injury (Taken from Kerin et al., 2022)
Proposed neural involvement
It has been suggested that a pattern of over-striding on the affected side could contribute to injury [5]. This blog proposes that the cause may be a combination of over-striding at the same time as ipsilaterally side flexing and rotating the trunk. This can result in compression of the spinal nerve roots as they exit the lateral recess of the vertebra, a position that has previously been linked to lumbar root symptoms [7]. Acute compression of the nerve roots which supply the sciatic nerve has been shown to influence the wide dynamic range (WDR) neuronal response [8]. With rapid inhibition following compression being shown to rapidly decrease the WDR response to noxious afferent stimuli. This view is supported by Topp & Boyd (2006) who suggest compression has been shown to cause structural alterations in myelin, which may result in impaired impulse conduction [9].
Nerves are routinely placed under stress and are able to accommodate this stress by gliding and elongating [9]. This stress can take the form of tensile, compressive or sheer combinations. All neural tissue will reach a point along its stress-strain curve whereby it transitions from a recoverable elastic strain to one which results in a plastic, or permanent deformation. If we relate this theory back to the proposed common injury mechanism, then a combination of compression at the proximal aspect of the sciatic nerve, followed by a tensile load generated by over-striding at the distal end of the nerve, could be theorised to result in a permanent plastic change in the neural structure. This could suggest why the reinjury rate is as high as 56% even with prolonged periods of rehabilitation [4], as we are looking for restoration in function in something other than musculotendinous tissue.
In an area where there is complex anatomy with dual innervation, it is vital that there is no interruption of the afferent or efferent impulses. Especially at the elite sporting level where any insufficiencies will likely result in subsequent injury.
Conclusion
- The high rate of reinjury around the T-junction suggests that there is another potential contributing factor to the injury
- It is proposed that if anecdotal injury mechanisms of ipsilateral trunk flexion correlate with distal musculotendinous biceps femoris injuries, then there may be an underlying neural contribution to the injury.
- This may explain why there is a high incidence of recurrence and therapists must consider appropriate rehabilitation strategies to address this potential contributing factor.
Authors: Adam Johnson (@PreventionPhys)- First Team Physiotherapist at Everton Football Club
No Competing Interests
Acknowledgments- I am a gold member of the Association of Chartered Physiotherapists in Sport (ACPSEM) and would like to acknowledge their support in the publication of this blog.
References
- Ekstrand, J., Bengtsson, H., Walden, M., Davison, M., Khan, K.K. & Hagglund, M. Hamstring injury rates have increased during recent seasons and now constitute 24% of all injuries in men’s professional football: the UEFA Elite Club Injury Study from 2001/02 to 2021/22. British Journal of Sports Medicine, 57, 292-298.
- Kenneally-Dabrowski, C., Serpell, B.G., Spratford, W., Lai. A.K.M., Field, B., Brown, N.A.T., Thomson, M. & Perriman, D. A retrospective analysis of hamstring injuries in elite rugby athletes: More severe injuries are likely to occur at the distal myofascial junction. Physical Therapy in Sport 2019, 38, 192-198.
- Entwisle, T., Ling, Y., Splatt, A., Brukner, P. & Connell, D. (2017). Distal Musculotendinous T Junction Injuries of the Biceps Femoris: An MRI Case Review. The Orthopaedic Journal of Sports Medicine 2017, 5(7), doi:10.1177/2325967117714998
- Shamji, R., James, S.L.J., Botchu, R., Khurniawan, K.A., Bhogal, G. & Rushton, A. Association of the British Athletic Muscle Injury Classification and anatomic location with retun to full training and reinjury following hamstring injury in elite football. BMJ Open Sport & Exercise Medicine 2021, 7(2), e001010.
- Kerin, F., Farrell, G., Tierney, P., Persson, U.K., De Vito, G. & Delahunt, E. (2022). Its not all about sprinting: mechanisms of acute hamstring strain injuries in professional male rugby union- A systematic visual video analysis. British Journal of Sports Medicine 2022, 56, 608-615.
- https://blogs.bmj.com/bjsm/2022/12/12/moving-towards-a-triplanar-view-of-hamstring-strain-injuries/
- Colak, A., Topuz, K., Kutlay, M., Kaya, S., Simsek, H., Cetinkal, A. & Demircan, M.N. A less invasive surgical approach in the lumbar lateral recess stenosis: Direct approach to the medial wall of the pedicle. European Spine Journal 2018, 17, 1745-1751.
- Wang, W., Tan, W., Luo, D., Lin, J., Yu, Y., Wang, Q., Zhao, W., Wu, B., Chen, J. & He J. Acute pressure on the sciatic nerve results in rapid inhibition of the wide dynamic range neuronal response. BMC Neuroscience 2012, 13, 147.
- Topp, K.S. & Boyd, B.S. Structure and Biomechanics of Peripheral Nerves: Nerve Responses to Physical Stresses and Implications for Physical Therapist Practice. Physical Therapy 2006, 86(1), 92-109.