How healthcare professionals can assess and manage arrhythmias in athletes without transient loss of consciousness using smart ECG devices.
Keywords: Athlete, Palpitations, ECG.
Introduction
Palpitations due to arrhythmias during sports can be a serious concern for athletes, and prompt assessment and management are crucial to ensure adequate diagnosis and treatment. As arrhythmias are time-sensitive and can potentially cause sudden cardiac death, timely assessment and management can help prevent adverse outcomes and allow athletes to continue their sports safely. In this blog post, we propose a guide for healthcare professionals to efficiently assess and manage athletes with palpitations using novel electrocardiography (ECG) devices, as there is currently a lack of guidance on using these devices in sports.
- Smart ECG device
Traditional approaches may not include rapid ECG assessment on the pitch. Smart ECG devices like smartwatches and portable ECG devices may provide single- or multi-lead ECGs [1,2]. These devices provide the healthcare professional the opportunity to obtain a real time assessment of a potential arrhythmia in an exercising athlete (see Figure 1 below).
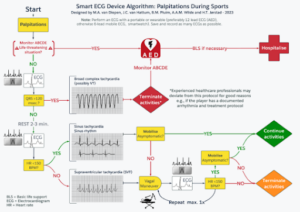
Figure 1: Smart ECG Device Algorithm for palpitations during sports
- First Assessment
Athletes who present with hemodynamic/respiratory instability or transient loss of consciousness require immediate assessment for basic life support and eventually connection to an AED [3]. In such cases, emergency response protocols should be initiated immediately. Hemodynamically/respiratory stable athletes can be preliminarily assessed by obtaining an ECG with a portable ECG device. We recommended using a device with multiple leads, but priority should be given to rapid assessment with the device available.
- Broad Complex Tachycardias
If the QRS is wider than 120 milliseconds on the ECG, the assumption should be that the athlete has ventricular tachycardia (VT) until proven otherwise [4,5]. Play should be stopped, and an AED should be applied. Emergency response protocols should be initiated. Experienced healthcare professionals may deviate from this protocol for justified reasons, e.g., if the player has a documented aberrant conducting supra ventricular tachycardia or a personalised treatment plan.
- Narrow Complex Tachycardias
If the ECG shows a narrow complex tachycardia (QRS shorter than 120 milliseconds), differentiation is warranted between sinus tachycardia and supraventricular tachycardia (SVT). A 2-to-3-minute resting period is central to this differentiation. If the narrow complex tachycardia persists after rest (> 150 beats per minute), we recommend performing a maximum of two modified Valsalva manoeuvres with passive leg elevation and supine positioning at the end of the manoeuvre (see video: Modified Valsalva manoeuvre for supraventricular tachycardia – YouTube) [6]. If the tachycardia does not persist or if terminated, the athlete should remain asymptomatic for palpitations during mobilization, before returning to sports.
- Recording and Documenting Arrhythmias
It is essential to record and document any arrhythmia for further diagnostic and management purposes. If digital documentation cannot easily or completely be obtained from the ECG device, healthcare professionals should strongly consider documenting arrhythmias, with the athlete’s consent, using smartphones or other devices with camera capability.
Conclusion:
Rapid assessment and management of arrhythmias in athletes are crucial to prevent adverse outcomes, but also to allow athletes to continue their sports safely. Our proposed step-by step guide, which utilizes novel smart and small ECG devices, can aid healthcare professionals in quickly assessing and managing palpitations on the pitch. By differentiating between broad and narrow complex tachycardias and performing vagal manoeuvres when appropriate, adverse outcomes can be prevented, and athletes can continue to pursue their sporting activities safely. We encourage healthcare professionals to consider incorporating our guide into their practice to improve the care of athletes with palpitations.

Author names & affiliations:
M.A. van Diepen, MD1 m.a.vandiepen@amsterdamumc.nl J.C. van Hattum, MD1 j.c.vanhattum@amsterdamumc.nl B.M. Pluim, MD PhD2,3,4 b.pluim@knltb.nl
C.A.C.M. Wijne, MD5 c.a.wijne@amsterdamumc.nl M.H. Moen, MD PhD6 maarten.moen@nocnsf.nl Prof. M. Börjesson, MD7 mats.borjesson@gu.se Prof. A.A.M. Wilde, MD PhD1 a.a.wilde@amsterdamumc.nl H.T. Jørstad, MD PhD1,8 h.t.jorstad@amsterdamumc.nl
1 Amsterdam UMC location University of Amsterdam, Department of Cardiology, Amsterdam, The Netherlands; Amsterdam Cardiovascular Sciences (ACS), Amsterdam, The Netherlands
2 Section Sports Medicine, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa
3 Amsterdam Collaboration on Health & Safety in Sports (ACHSS), IOC Research Centre of Excellence, Amsterdam, the Netherlands
4 Medical Department, Royal Netherlands Lawn Tennis Association (KNLTB), Amstelveen, the Netherlands
5 Sports Physicians, OLVG Location West, Amsterdam, The Netherlands
6 Dutch Olympic Committee*Dutch Sports Federation (NOC*NSF) High Performance Team
7 Inst Medicine, Sahlgrenska Academy, Gothenburg University and Sahlgrenska University Hospital, Gothenburg, Sweden
8 Amsterdam Movement Sciences (AMS), Amsterdam, The Netherlands
Competing Interests:
The authors declare no competing interests.
References:
1. Jewson JL, Orchard JW, Semsarian C, et al. Use of a smartphone electrocardiogram to diagnose arrhythmias during exercise in athletes: a case series. Eur Heart J Case Rep 2022;6:ytac126. doi:10.1093/ehjcr/ytac126
2. Kassam N, Aziz O, Aghan E, et al. Smart Watch Detection of Supraventricular Tachycardia (SVT): First Case from Tanzania. Int Med Case Rep J 2021;Volume 14:563– 6. doi:10.2147/IMCRJ.S328167
3. de Jong JS, Jorstad HT, Thijs RD, et al. How to recognise sudden cardiac arrest on the pitch. Br J Sports Med 2020;54:1178–80. doi:10.1136/bjsports-2019-101159
4.Ringwald M, Crich A, Beysard N. Smart watch recording of ventricular tachycardia: Case study. Am J Emerg Med 2020;38:849.e3-849.e5. doi:10.1016/j.ajem.2019.10.040
5.Burke J, Haigney MCP, Borne R, et al. Smartwatch detection of ventricular tachycardia: Case series. HeartRhythm Case Rep 2020;6:800–4. doi:10.1016/j.hrcr.2020.08.003
6. Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J 2020;41:655–720. doi:10.1093/eurheartj/ehz467