Author: Georgios Kakavas PT OMT PhD
Introduction
Tendinopathy remains one of the most persistent and challenging conditions in sports medicine. Traditional rehabilitation often emphasizes tendon loading and strength training but may overlook central nervous system adaptations that affect movement control, pain perception, and long-term outcomes.
A new evidence-based framework, called neuroplastic periodization, proposes a holistic, structured approach to tendon rehab that integrates both peripheral tissue healing and central motor learning (1). Despite the growing body of research on tendinopathy rehabilitation, there remains a gap in the literature regarding the systematic application of structured periodization approaches. Current rehabilitation protocols often lack a cohesive framework that balances load progression, recovery, and performance optimization in a way that aligns with the tendon’s capacity for adaptation (2).
This blog provides information to clinicians about this new concept of neuroplastic periodization of tendinopathy rehabilitation.
Why Neuroplasticity Matters in Tendon Rehab
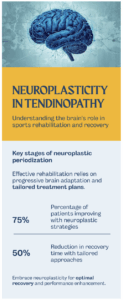
Injury to tendons often leads to disrupted motor control, including altered motor unit activation, cortical excitability, and compensatory y-movement patterns in the contralateral limb. These maladaptive neural changes can persist even after the tendon healing has started, increasing the risk of re-injury or chronic pain. Therefore,rehabilitation should not focus exclusively on the local tissue. Neuroplastic periodization emphasizes the role of modifications in nervous system function as a key driver of recovery (3) (see Figure 1).
Figure 1: Neuroplastic rehabilitation phases according to G. Kakavas et al. (2025)
Phases of the Neuroplastic Rehabilitation
- Pain Modulation & Neuromuscular Priming: Use high-duration isometric holds (e.g., heavy sustained contractions) to reduce pain and enhance motor unit recruitment (3).
- Progressive Heavy‑Slow Resistance (HSR): Resistance exercises stimulate tendon remodeling and build strength, following a phased periodization model.
- Neuromotor Control & Power Integration: Introduce externally paced, sport-specific movements to reinforce corticospinal drive and improve coordination (4).
Beyond Exercise: The Neurocognitive Component
A distinctive aspect of this model is the incorporation of neurocognitive strategies, including tasks that engage motor learning and attention, such as visual feedback, varied movement contexts, or dual-task drills. These elements foster stronger brain–body integration and adaptive movement patterns (5).
Implementation Guidelines for Clinicians
The new guidelines for clinicians must provide holistic tendon care, which must include:
- Assess the kinetic chain thoroughly (ROM, tissue flexibility, biomechanics, and neuromuscular symmetry).
- Progress based on functional benchmarks: aim for symmetrical strength, pain-free tasks, and load tolerance.
- Adjust variables intentionally: sets, reps, load, contraction mode, pacing, and movement variability (6).
Theoretical Roadmap for Neuro-Rehabilitation Goals
- Pain control. Sustained isometrics (e.g., 45s hold × 4) | Internal focus: Both are needed for pain management in tendinopathy sufferers.
- Strengthening. Heavy-slow concentric/eccentric | External pacing: Those components are critical for strengthening the tissue
- Power & coordination. Sport-specific drills | Dual-task: This combination is vital for power, coordination, and RTS.
What Research Still Needs to Be Done?
There are currently no randomized controlled trials testing neuroplastic periodization in tendinopathy. Future studies and clinicians should focus on comparing this approach with conventional protocols and conduct long-term follow-ups of function, re-injury, and patient-reported outcomes.
Conclusion
Neuroplastic periodization represents a forward-thinking, blended approach to tendon rehabilitation. By combining progressive loading, neurocognitive training, and structured periodization, this model aims to restore tendon resilience and neuromotor control, ultimately leading to better pain resolution, movement quality, and long-term recovery.
References
- Kakavas G, Forelli F, Korakakis V, Malliaropoulos N, Maffulli N. Neuroplastic periodization in tendinopathy. Br Med Bull. 2025 Apr 4;154(1):ldaf006. doi: 10.1093/bmb/ldaf006. PMID: 40455651.
- Khan KM, Cook JL, Bonar F, Harcourt P, Strom M. Histopathology of Common Tendinopathies: Update and Implications for Clinical Management. Sports Med. 1999;27(6):393–408.
- Abate M, Gravare-Silbernagel K, Siljeholm C, Di Iorio A, De Amicis D, Salini V, et al. Pathogenesis of tendinopathies: inflammation or degeneration? Arthritis Res Ther. 2009;11(3):235.
- Rees JD, Stride M, Scott A. Tendons – time to revisit inflammation. Br J Sports Med. 2014 Nov;48(21):1553–7.
- Maffulli N. Overuse tendon conditions: Time to change a confusing terminology. Arthrosc J Arthrosc Relat Surg. 1998 Nov;14(8):840–3.
- Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015 Oct;49(19):1277–83.