Author: Jamon Couch
We recently published our systematic review in BJSM investigating the prevalence of knee crepitus and its association with structural pathology among the general population and across knee conditions. The summary of this study is outlined in this blog.
Why is this study important?
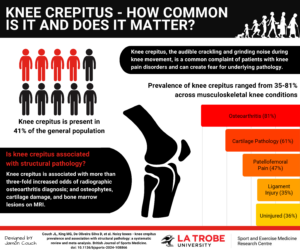
Knee crepitus, the audible crackling or grinding noise during knee joint movement, can be experienced across the lifespan and create fear for underlying pathology.1-4 While some studies suggest that knee crepitus is benign,2-4 others have found the presence of crepitus to be an early clinical indication of underlying structural knee pathology, such as osteoarthritis (OA).5 The purported association between knee crepitus and radiographic OA has led to international guidelines endorsing crepitus as a key clinical diagnostic feature of knee OA.6,7 However, knee crepitus is also observed in people without pain or underlying pathology,8,9 provoking debate about the diagnostic value of this clinical sign.8
Patients often describe catastrophising beliefs around their knee crepitus, negatively impacting their engagement with physical activity, occupation, and even rehabilitation. Patients also report that consulting a health practitioner about their knee crepitus is a negative experience, with many feeling their concerns are inadequately addressed.10 A reliable estimate of knee crepitus prevalence in the general population and across different knee conditions, and its association with underlying structural pathology, is important to determine its clinical significance.
How did the study go about this?
This systematic review and meta-analysis was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidance. We evaluated studies reporting the prevalence of knee crepitus and its association with structural pathology on medical imaging. Crepitus prevalence estimates were calculated by pooling data based on knee condition using random-effects proportion meta-analysis. Meta-analyses to determine the association between crepitus and structural pathology were conducted using random-effects models. Best-evidence synthesis complemented meta-analyses when a lack of data precluded meta-analysis
What did the study find?
103 studies involving 36,439 participants (42,816 knees) revealed that knee crepitus is common amongst those with, and without, a musculoskeletal knee condition. Most studies assessed crepitus using physical examination methods. Knee crepitus is present in 41% of the general population, 36% in uninjured pain-free controls, 81% in knee osteoarthritis, and ranges from 35% to 61% in other musculoskeletal knee conditions. The presence of knee crepitus was associated with a more than three-fold increased odds of radiographic osteoarthritis diagnosis. Knee crepitus is also associated with the presence of osteophytes, cartilage damage, and bone marrow lesions on magnetic resonance imaging.
What are the key take-home points?
Knee crepitus is present in almost half of the general population and over one-third of those without a history of knee injury.
Knee crepitus is common across a number of musculoskeletal knee conditions, but is most prevalent in those with diagnosed knee OA.
The presence of knee crepitus is associated with more than three-fold increased odds of radiographic osteoarthritis diagnosis and several imaging-based structural osteoarthritis features.
On the weight of available data, patients presenting with knee crepitus should be counselled that this clinical sign is common across the general population, and despite being associated with underlying structural pathology, may not be a direct cause for concern.
References
- Crema MD, Guermazi A, Sayre EC, et al. The association of magnetic resonance imaging (MRI)-detected structural pathology of the knee with crepitus in a population-based cohort with knee pain: the MoDEKO study. Osteoarthritis and cartilage. 2011;19(12):1429-1432. doi:10.1016/j.joca.2011.09.003
- de Oliveira Silva D, Barton C, Crossley K, et al. Implications of knee crepitus to the overall clinical presentation of women with and without patellofemoral pain. Physical therapy in sport. 2018;33:89-95. doi:10.1016/j.ptsp.2018.07.007
- de Oliveira Silva D, Pazzinatto MF, Priore LBD, et al. Knee crepitus is prevalent in women with patellofemoral pain, but is not related with function, physical activity and pain. Physical therapy in sport. 2018;33:7-11. doi:10.1016/j.ptsp.2018.06.002
- Pazzinatto MF, de Oliveira Silva D, Azevedo FMd, Pappas E. Knee crepitus is not associated with the occurrence of total knee replacement in knee osteoarthritis – a longitudinal study with data from the Osteoarthritis Initiative. Revista brasileira de fisioterapia (São Carlos (São Paulo, Brazil)). 2019;23(4):329-336. doi:10.1016/j.bjpt.2018.09.009
- Schiphof D, van Middelkoop M, de Klerk BM, et al. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis). Osteoarthritis and cartilage. 2014;22(5):631-638. doi:10.1016/j.joca.2014.02.008
- Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis and rheumatism. 1986;29(8):1039-1049. doi:10.1002/art.1780290816
- Zhang W, Doherty M, Peat G, et al. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Annals of the Rheumatic Diseases. 2010;69(3):483-489. doi:10.1136/ard.2009.113100
- Johnson LL, van Dyk GE, Green JR, et al. Clinical assessment of asymptomatic knees: comparison of men and women. Arthroscopy. 1998;14(4):347-359. doi:10.1016/S0749-8063(98)70001-5
- McCoy GF, McCrea JD, Beverland DE, Kernohan WG, Mollan RAB. Vibration arthrography as a diagnostic aid in diseases of the knee. Journal of bone and joint surgery British volume. 1987;69(2):288-293.
- Robertson CJMPM, Hurley MP, Jones FP. People’s beliefs about the meaning of crepitus in patellofemoral pain and the impact of these beliefs on their behaviour: A qualitative study. Musculoskeletal science & practice. 2017;28:59-64. doi:10.1016/j.msksp.2017.01.012