Unpicking hip pain in young athletes; pincers & bump: FAI syndrome or just an athletic hip?
Introduction
Young athletes often complain of groin pain. When pain originates from the hip joint, clinicians refer to it as hip-joint related groin pain. Hip-joint related groin pain can cause significant time loss at a key stage of development and training in young athletes. Recent consensus statements have helped to define a framework for assessing hip-related groin pain in athletes and help sports medicine clinicians to work up, image and manage patients with ‘Femoroacetabular Impingement (FAI) Syndrome’ – one of the conditions causing hip-related groin pain. We discuss current concepts around the management of patients with FAI syndrome, and if this is just a normal bump, symptomatic pathology, and the early opportunity to detect impingement in order to prevent osteoarthritis (OA) developing in later life.
A consensus on the athlete’s hip
In 2016, the first international consensus statement (Warwick) was designed to help create a definition of FAI syndrome in athletes. It described the key triad of: symptoms, clinical signs and imaging findings found in athletes that are exposed to extreme repetitive physiological stresses of the hip (ball and socket joint) and soft tissues. Since then further consensus statements (Oxford, involving a much larger and more diverse expert panel), refined the Warwick consensus terminology and helped to define areas for future research in the young athletic hip. The ESSKA 2024 consensus on Hip and Groin Pain (1) built on several recent consensus studies (including four Zurich Consensus papers and two Oxford Consensus papers – see below) to cement the standard use of the term FAI syndrome, categorising it as a type of hip-joint related groin pain. There is a significant overlap between patients with changes in the shape of the hip with no pain and those that are symptomatic and need intervention. This spectrum of presentations highlights the importance of referring to the ‘morphology’ of the hip in cam/pincer impingement, and not ‘abnormalities’ or ‘lesions’.
| Subtypes | What does that look like? | Prevalence |
| Cam Morphology
A bony bump at the junction between the ball and neck in the ball and socket joint (aspheric femoral head). |
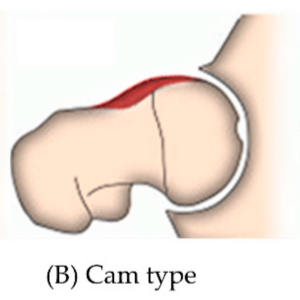 |
Some studies report cam morphology may be present in around 66% of athletes (2).
Most common in young, athletic males (3), although more research is required in female athletes. |
| Pincer Morphology
A deep socket in the ball and socket joint (deep acetabulum). |
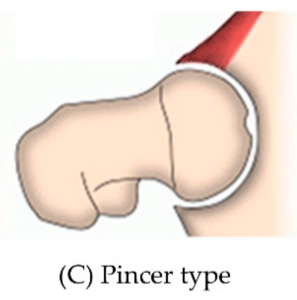 |
Some studies report pincer morphology may be present in around 51% of athletes (2).
Most common in middle-aged females (3). |
| Mixed Morphology
A combination of the ball and socket morphology as described above. |
 |
Mixed morphology is reported to be present in around 57% of athletes in some studies (2).
Often thought to be the most common subtype (4). |
Table 1: Subtypes of FAIS (Image source (5))

Figure 1: Cam morphology compared to the contour of a pistol’s grip, in reference to the now outdated term ‘pistol grip deformity’ (6).
FAI syndrome and sports participation
Although our understanding of the exact relationship between hip morphology and sports participation is still developing, many studies have shown that athletes have a higher prevalence of primary cam morphology (and likely pincer morphology too) compared to the general population.
| General Population | Cam Morphology Incidence | Pincer Morphology Incidence | Mixed Cam/Pincer Morphology Incidence |
| Symptomatic | 17% | 18% | 65% |
| Asymptomatic | 37% | 67% | 36% |
Table 2: Incidence rates of FAIS subtypes in the general population (7-9)
The risk of primary cam morphology (and FAI syndrome) varies by sports with higher cumulative stresses on the hip particularly during adolescent years seen as a key risk factor. Primary cam morphology is usually only seen (on x-rays, and earlier on MRI) after the age of 13 in boys (and likely earlier in girls), when closure of the growth plates starts to commence (10). Participation in academy or professional sport increases the incidence of cam morphology and symptoms (2-3x) compared to controls (11). Understanding the risk factors contributing to FAI syndrome and an awareness of how these may develop in a sportsmen/women therefore becomes essential to the clinicians responsible for delivering education, symptomatic care and management especially in the younger population of active individuals.
Sport-related factors contributing to FAI syndrome:
- Repetitive stresses from sports as an adolescent (12)
- Higher frequency training
- Higher level of sport
- Professional or academy status
| Sport Type | Cam Morphology Prevalence | Pincer Morphology Prevalence | Mixed Morphology Prevalence |
| Rowing | 48% | 0% | 24% |
| Ice Hockey | 41% | 10% | 10% |
| Gaelic Football | 100% | – | 72% |
| Baseball | 55% | 47% | 34% |
| Golf | 16% | 0% | – |
| Football | 53% | 20% | 32% |
| Ballet | 18% | 58% | – |
| Track & Field | 50% | 9% | 5% |
| American Football | 73% | 54% | 63% |
| Capoeira | 92% | 38% | 33% |
Table 3: Prevalence of FAIS subtypes by sport (Table data source (13)).
Radiological findings (X-Ray changes) suggestive of cam/pincer morphology have a significant overlap and are often seen in many asymptomatic patients. As a result, radiographic changes alone may be considered ’normal’ and does not require further treatment in the absence of clinical symptoms (14).
A sports physician’s dilemma; Unpicking asymptomatic x-ray changes (morphology) from the painful hip (FAI syndrome)
This can be tricky and sports medicine physicians will need to work up the patient with a clear
history and examination, to determine the pre-test possibility of the athlete having FAI syndrome before interpreting imaging findings. The most common features to enquire about are:
- Insidious onset anterior hip/buttock/back or thigh pain,
- Pain made worse by physical activity.
- Pain on activities requiring hip flexion and rotation,
- Hip stiffness or difficulty when stretching.

Figure 2: Summary of presenting, characteristic features of FAIS.
| Biomechanical | Medical |
|
|
Table 4: Biomechanical and medical risk factors for FAIS (15,16).
Diagnosing FAI syndrome
The Warwick Agreement (17) has outlined guidance on how to diagnose FAI syndrome. Diagnosis requires three components: appropriate symptoms, clinical signs and radiographic evidence consistent with the disorder.
Where there are radiographic changes and equivocal symptoms – then a diagnostic intra articular joint injection can be considered to confirm the diagnosis. This can be guided either by ultrasound or fluoroscopy and can reliably distinguish intra-articular from extra-articular pathology.
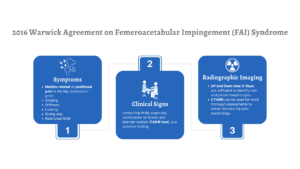
Figure 3: Infographic of the 3 criteria required to diagnose FAI, as per the 2016 Warwick Agreement.
The primary symptoms are:
- Motion-related or positional pain in the hip, buttocks or groin
- Clicking, stiffness, locking, giving way
- Restricted range of motion
When patients present with hip pain, it is crucial not to overlook the potential for serious pathology, especially if their symptoms do not align with common clinical entities like adductor, inguinal, iliopsoas, pubic, or hip-related groin pain. Red flags that may indicate a non-musculoskeletal cause include unexplained weight loss, night pain, fever, a history of cancer, or neurological deficits.
If serious pathology is suspected, referring the patient to an appropriate specialist for further evaluation and management is critical.
Clinical signs
All suspected cases require systematic clinical examination of the hip and groin. In particular, hip range of motion and a FADIR test should be utilised. If they provoke pain, this increases the probability of hip pathology and FAI syndrome.
Range of motion should also be assessed in the prone position due to rotational and version variances of the femur and tibia.
- Flexion adduction internal rotation (FADIR)
- Flexion abduction external rotation (FABER)
- Limited hip range of motion or pain in maximal internal rotation with overpressure
| Clinical Test | Positive Result | Sensitivity | Specificity |
| Flexion adduction internal rotation (FADIR) | This position recreates groin pain | 96% | 11% |
| Flexion abduction external rotation (FABER) | Recreates groin pain and/or hip ROM is limited | 89% | 97% |
| Internal rotation over pressure (IROP) | Recreates groin pain | 88% | 17% |
Table 5: Summary of clinical tests for FAIS, including their sensitivity and specificity (18-21).

Figure 4: Flexion adduction internal rotation (FADIR) clinical test.

Figure 5: Flexion abduction external rotation (FABER) clinical test.

Figure 6: Internal rotation over pressure (IROP) clinical test.
MSK imaging
- AP and Dunn view (or similar lateral view) x-rays of the hips are sufficient for diagnosis
- If further definition is required of the soft tissues (labrum, cartilage or surrounding musculature) then MRI can be considered and is 2nd line for further assessment
- Cross-sectional imaging CT can be used to model the acetabulum/femoral head for planning orthopaedic intervention but should be used with caution to due to the ionising radiation
- Ultrasound can be used to screen for key features in cam morphology FAI syndrome with high sensitivity (81-93%) and specificity (82-88%), but is operator dependent
| X-ray |
|
First line imaging and usually sufficient for diagnosis (22). |
| MRI |
|
Particularly good for detecting soft tissue/cartilage/labrum injury (22). |
| CT |
|
Involves ionising radiation, although low dose protocols can be used for 3D modelling during surgical planning (1). |
| US |
|
Quick and relatively inexpensive, although operator dependent. |
Table 6: Summary of the radiographic features for FAIS across various imaging modalities.
Key terms to look out for in a radiology report that may indicate FAI syndrome include:
- Femoral head-neck bumps, cysts, herniation pit
- Femoral head-neck offset ratio < 0.17
- Alpha angle ≥ 60° indicates cam morphology (or primary cam morphology in the young athlete with no previous history of hip disease)
- Acetabular index < 3°
- Lateral Centre-Edge Angle (LCEA) > 39°
- Anterior Femoral Distance > 4mm
- Acetabular retroversion
- Femoral anteversion
- Resultant labral damage and chondral lesions
- Signs of early onset osteoarthritis (subchondral cysts, sclerosis, osteophytes)


Figure 8: Infographic highlighting key radiological features of FAIS.
Treatment options
Although nonoperative and operative treatment options exist for FAI syndrome, there is no consensus on standardised treatment algorithms. Treatment options should be considered with individual risk factors, and sport-specific considerations as part of a shared decision-making approach.
Similarly, there is no consensus on a physiotherapy programme, including clinician-led incremental exercise rehabilitation and education, which directly improves FAI syndrome symptoms. Strategies tend to focus on hip strengthening, mobility and neuromuscular control (23). When physiotherapy has been advised it has generally focused on improving the hip muscle flexibility and core strength with a staged approach in order to reduce the impingement frequency.
| Non operative options | Operative options |
|
|
Table 7: Overview of the operative and non operative management options for FAIS.
Patient education plays a key role in both aspects of nonoperative and operative management. Initial educational interventions should aim to help patients modify their daily activity involving the hips e.g. walking, sitting etc, whilst avoidance of aggravating factors e.g crossing legs or pivoting can all contribute to symptom control prior to any conversations on operative management.
Validated, patient-reported outcome measures should be used to assess treatment effectiveness, such as (17):
- International Hip Outcome Tool (iHOT)
- Hip and Groin Outcome Score (HAGOS)
- Hip Outcome Score (HOS)
Tailoring your approach to treatment
Data on a range of non-surgical and surgical treatments have been published for FAI syndrome, but inclusion and diagnostic criteria has varied across studies. A recent (Oxford) consensus statement has outlined areas for future research and imaging criteria to define cam morphology for research purposes and prospective studies (24).
When deciding on treatment options for FAI syndrome, clinicians must consider:
- There are high rates of “cam morphology” in asymptomatic patients.
- Pain symptoms can vary with loading/use of the hip in provocative motions.
- Negative labels such as “lesion”, “bump” or “hip abnormality” can have an impact on a patient’s perception of the condition. Clinicians should avoid these terms.
- FAI syndrome represents a spectrum of changes: cam, pincer or mixed morphology.
- In some patient’s the changes seen in the labrum and cartilage surfaces with FAI syndrome may predispose patients to early onset osteoarthritis.
Conclusion
- FAI syndrome requires a triad for diagnosis – symptoms, clinical signs and radiographic findings. This helps differentiate between variation and pathology.
- AP and Dunn view x-rays are sufficient to detect radiographic features and diagnose FAI syndrome.
- Ultrasound is an exciting new imaging modality, especially in screening for key FAI syndrome features
- Treatment should be individual-specific and involve shared decision making.
Supplementary Infographic on radiographic features:
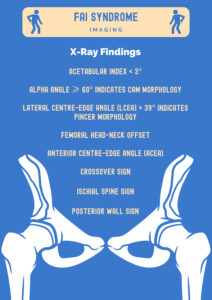
Figure 9: Supplementary infographic highlighting some of the key x-ray findings characteristic of FAIS.
Authors & Affiliations:
Dr Isa Waheed, Dr Rifat Hassan, Muhammad Umer, Dr Ryan Linn, Dr Irfan Ahmed, Mr Mark Moriarty, Dr Imran Lasker, Dr Paul Dijkstra.
Dr Isa Waheed
Foundation Year 2 Doctor
London North West Healthcare Trust
Insta: @drisawaheed
Dr Rifat Hassan
Foundation Year 2 Doctor
Norfolk & Norwich University Hospitals
Insta: @RifatHassan_
Muhammad Umer
5th Year Medical Student
King’s College London
Dr Ryan Linn
Foundation Year 1 Doctor
University Hospitals of North Midlands
X: @Ryan_Linn_
Dr Irfan Ahmed
Consultant in Musculoskeletal, Sport & Exercise Medicine
Website : www.mskplaybook.com
Mr Mark Moriarty
Health advisor
BUPA St Albans
Dr Imran Lasker
Consultant Radiologist with Special Interest in MSK
Mid & South Essex Foundation Trust
X: @DocLasker
Links to MSK/MRI courses: imranlasker.com, radiologyseminars.com. emergencyimaging.co.uk
Dr Paul Dijkstra
Consultant Sport and Exercise Medicine Physician
Director of Medical Education at Aspetar, Qatar – Orthopaedic and Sports Medicine Hospital
Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences
Bibliography
1 – Hip and Groin Pain in Physically Active Adults A Formal ESSKA-EHPA-ESMA Consensus [Internet]. [cited 2024 Jul 28]. Available from: https://cdn.ymaws.com/www.esska.org/resource/resmgr/docs/consensus_projects/2024_groin_summary.pdf
2 – Mascarenhas VV, Rego P, Dantas P, Morais F, McWilliams J, Collado D, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: A systematic review. European Journal of Radiology [Internet]. 2016 Jan [cited 2019 Dec 11];85(1):73–95. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0720048X15301364
3 – Silvers HJ, Giza E, Jolly J. The relationship of gender, age, and ethnicity to incidence of anterior cruciate ligament reconstruction in athletes. J Orthop Sports Phys Ther. 2006;36(1):34-9. Available from: https://www.jospt.org/doi/10.2519/jospt.2006.2135
4 – Culvenor AG, Alexander I, Mackay M, Collins NJ, Khan KM, Crossley KM. Risk factors for knee osteoarthritis in former elite female athletes. BMC Musculoskelet Disord. 2022;23:650. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9404268/
5 – Waarsing JH, van Ganz R, Reijman M, Bierma-Zeinstra SMA, Verhaar JAN. The symptomatic FAI group demonstrated. Healthcare. 2022;10(8):1484. Available from: https://www.mdpi.com/2227-9032/10/8/1484#:~:text=The%20symptomatic%20FAI%20group%20demonstrated,in%20both%20men%20and%20women.
6 – O’Connor PJ, Laws CJ, Bloem RM, Kavanagh EC. Symptomatic lumbar disk disease in adult patients with spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 2008;90(10):2234-43. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2505145/
7 – Briggs KK, Philippon MJ, Ho CP, Hurwitz S, Steadman JR. Prevalence of acetabular dysplasia and preoperative factors associated with clinical outcome following arthroscopic labral refixation in patients with femoroacetabular impingement. Orthop J Sports Med. 2013;1(4):2325967113510841. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3049607/#:~:text=Numerous%20plain%20radiographic%20findings%20have,retroversion%20%5B3%2C%208%5D.
8 – Sierra RJ, Beaule PE, Zaltz I, Clohisy JC. Outcomes of joint-preserving surgery for femoroacetabular impingement: a systematic review of the literature. J Arthroplasty. 2014;29(9):182-7. Available from: https://www.sciencedirect.com/science/article/pii/S0749806314009682?via%3Dihub
9 – Palmer WE, Afonso L, Brown J, Rosenthal DI. Incidence of radiographic findings of femoroacetabular impingement in asymptomatic subjects. Orthop Pract. 2021;32(1):43-7. Available from: https://journals.lww.com/c-orthopaedicpractice/Fulltext/2021/01000/Incidence_of_radiographic_findings_of.6.aspx
10 – Kim YJ, Novais EN, Johnson VM, Wells L, Millis MB, Kim KM. The prevalence of radiographic findings of femoroacetabular impingement in a young asymptomatic population. Am J Sports Med. 2012;40(10):2248-54. Available from: https://pubmed.ncbi.nlm.nih.gov/22415206/
11 – Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study. Am J Sports Med. 2013;41(3):587-93. Available from: https://pubmed.ncbi.nlm.nih.gov/22343678/#:~:text=Results%3A%20In%20total%2C%2072%25,evidence%20of%20radiographic%20hip%20abnormality.
12 – Botser IB, Smith TW, Nasser R, Domb BG. Femoroacetabular impingement: pathophysiology and diagnosis. Orthopedics. 2012;35(3):223-30. Available from: https://pubmed.ncbi.nlm.nih.gov/22354406/
13 – Alradwan H, Philippon MJ, Farrokhyar F, Chu R, Sobolev B, Whelan DB. Return to sport after surgical management of femoroacetabular impingement in athletes: a systematic review. Am J Sports Med. 2021;49(5):1290-6. Available from: https://journals.sagepub.com/doi/10.1177/03635465211023500#fig5-03635465211023500
14 – Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-20. Available from: https://journals.lww.com/clinorthop/fulltext/2003/12000/femoroacetabular_impingement__a_cause_for.13.aspx
15 – Harris JD, Siston RA, Pan X, Michalski MP, Davis BR, Flanigan DC. Treatment of femoroacetabular impingement: a systematic review. Curr Rev Musculoskelet Med. 2015;8(2):120-7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4513226/
16 – Jeng C, Tang H, Liu Y, Liu S. The epidemiology of femoroacetabular impingement. Hip Int. 2014;24(3):245-53. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3931341/
17 – Sogbein OA, Shah A, Kay J, Memon M, Simunovic N, Ayeni OR. Hip arthroscopy in patients with femoroacetabular impingement and borderline hip dysplasia: a systematic review. Br J Sports Med. 2016;50(19):1169-76. Available from: https://bjsm.bmj.com/content/50/19/1169.long
18 – Memon M, Kay J, Hache P, Simunovic N, Duong A, Ayeni OR. Hip arthroscopy for femoroacetabular impingement with capsular management: a systematic review. Orthop J Sports Med. 2020;8(4):2325967119898447. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213881/
19 – Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage. Hip Int. 2004;14(Suppl 3):11-2. Available from: https://pubmed.ncbi.nlm.nih.gov/12792209/
20 – Kemp JL, Makdissi M, Schache AG, Finch CF, Pritchard MG, Crossley KM. Hip chondropathy at arthroscopy: prevalence and relationship to labral pathology, femoroacetabular impingement, and patient-reported outcomes. Osteoarthritis Cartilage. 2014;22(3):378-85. Available from: https://www.oarsijournal.com/article/S1063-4584(15)01059-6/fulltext
21 – Memon M, Kay J, Hache P, Simunovic N, Duong A, Ayeni OR. Hip arthroscopy for femoroacetabular impingement with capsular management: a systematic review. Orthop J Sports Med. 2016;8(4):2325967119898447. Available from: https://pubmed.ncbi.nlm.nih.gov/20359681/
22 – Khan W, Zahar A, Muntaseer MA. Femoroacetabular impingement syndrome. Radiopaedia. 2024. Available from: https://radiopaedia.org/articles/femoroacetabular-impingement-syndrome?lang=gb
23 – Wall PDH, Fernandez M, Griffin DR, Foster NE. Nonoperative Treatment for Femoroacetabular Impingement: A Systematic Review of the Literature. PM&R [Internet]. 2013 Feb 15;5(5):418–26. Available from: https://www.sciencedirect.com/science/article/pii/S1934148213000865
24 – Dijkstra H, Sean Mc Auliffe, Ardern CL, Kemp JL, Mosler AB, Price A, et al. Oxford consensus on primary cam morphology and femoroacetabular impingement syndrome: part 1—definitions, terminology, taxonomy and imaging outcomes. British Journal of Sports Medicine. 2022 Dec 6;bjsports-106085.