Keywords: Collision Sport; Sports Therapy
Introduction
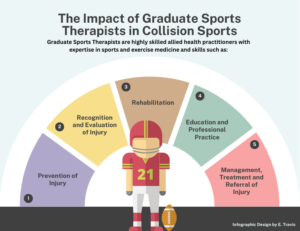
Since its formation in 1990, members of the Society of Sports Therapists (SST) have become valued practitioners within the allied healthcare profession pool and integral members of medical teams within sport (1). Graduate Sports Therapists (GSTs), who have successfully completed one of the 40 SST accredited undergraduate or postgraduate programmes, have gained skills aligned to 5 pillars of competency: prevention of injury; recognition and evaluation of injury; management, treatment, and referral of injury; rehabilitation and education and professional practice Issues (2). GSTs are skilled in these five areas, providing high-quality musculoskeletal care to athletic populations.
One of the key areas sitting across all 5 pillars of competency is trauma management, which includes skills such as administering pitch-side emergency trauma first-aid in competitive sporting environments and the recognition and management of life and limb threatening injuries/conditions. In collision sports such as American Football, Rugby Union and Ice Hockey, athletes are exposed to severe and often traumatic injuries such as fractures, sports-related concussion, facial injuries, and internal organ injuries (3, 4). GSTs are therefore ideally placed to be present and responsive in sports trauma situations within collision sports. This skill set is acknowledged by governing bodies such as the English Football Association and England Rugby, who recognise GST s as appropriate delegates on their pre-hospital trauma management courses; often a pre-requisite for employment in full time sport. The importance of this skill set was recognised by Martin (5), in response to Waddington et al. (6), who highlighted that medical practitioners with speciality and experience should be present in sports settings, if medical litigation and safeguarding issues are to be avoided.
Below outlines how GSTs skills support the collision sport athlete during trauma situations.
Prevention of injury
Injuries in collision sports can lead to time loss that can set the athlete back both mentally and physically (7,8). GST’s have the knowledge to aid injury prevention and illness risk factor identification across a multitude of sports. Examples include providing warm up, cool-down and recovery strategies; ensuring the correct fitting and maintenance of protective equipment; carrying out appropriate physical screening assessments; understanding the aetiology and epidemiology of sports; implementing exercise prescription and applying athletic strapping. Through this comprehensive and multi-faceted support, the athlete can have confidence in their readiness to participate in sport.
Recognition and Evaluation of Injury
In a collision sport environment, GSTs are skilled in their ability to carry out appropriate initial assessments. Injury assessments may take place in a variety of environments, from pitch to a clinic. Initial assessments provide the opportunity for a GST to identify and diagnose the problem through strong understanding of injury epidemiology. Examples of assessment include the ability to recognise medical emergencies such as sports-related concussion, maxilla-fascial injuries, diabetic or asthmatic emergencies and Sudden Cardiac Arrest.
Management, Treatment and Referral of injury
Timely management of injuries and medical emergencies in collision sports is crucial to a successful health outcome and return to sport. Lenjani et al. (9) noted that on the football field, and in other sports, a rapid approach was required when managing minor or multiple injuries at pre-hospital and hospital level with the provision of optimal medical care. GSTs are skilled in the management of potentially severe musculoskeletal injuries, spinal injuries, where careful and precise immobilisation is required to remove an athlete from a competitive sporting environment. If necessary, in collision-based sports where the athlete is wearing equipment, GSTs are required to carry the tools to remove such equipment and be skilled in the ability to do so. Coordination of medical actions from an experienced multidisciplinary team is required to avoid delays in the management of injury and illness on the field of play (9). As GSTs commonly work as part of a wider multidisciplinary team, they understand appropriate referral pathways to best serve the injured athlete. Additionally, GSTs understand the ethical and legal requirements in maintaining medical records, including the documentation of the management, treatment, and referral of medical emergencies.
Rehabilitation
Where an athlete can return to the field of play, the GST is well placed to understand the sport specific needs of the athlete, due to their training in physiology, biomechanics, and exercise prescription. This allows for tailored sport-specific drills and activities to be devised to ensure the athlete can meet the physical demands of the sport upon return to play. Knowledge related to rehabilitation is inclusive of musculoskeletal injuries (i.e., sprains, strains, fractures, haematomas etc) and sports-related concussions.
Education and Professional Practice Issues
GSTs frequently educate and support athletes, coaches, parents/guardians as part of the injury prevention or management process. Examples of this may be highlighting recovery strategies, injury risk reduction methods and doping regulations. Furthermore, GSTs can provide further team support for wider injury management practices including the implementation of medical emergency action plans/procedures and risk assessments. Implementation of these can be put in place through the training of team management, coaches, and other health care professionals. Enhancing the knowledge of individuals involved in sport promotes a safer training and competitive environment. In addition to these granular level activities, GST s work as consultants with governing bodies, specifically tasked with policy and procedure surrounding medical provision.
To conclude, GSTs are highly skilled allied health practitioners with expertise in sport and exercise medicine. Their specific skills upon the point of qualification in trauma management make them attractive to work in collision-based sports where severe and life-threatening injury is expected. Their knowledge of safely returning athletes to pre-injury state should see them be viewed as a valuable member of any sporting multidisciplinary team.
Authors:
Eleanor Travis – School of Health, Leeds Beckett University, UK
Dr Ashley Jones – School of Health, Leeds Beckett University, UK
Jodie Bennett – School of Health, Leeds Beckett University, UK
Helen Llewellyn – School of Health, Leeds Beckett University, UK
Competing Interests:
All authors deliver on a Sport and Exercise Therapy degree programme.
References
- Smith, G.N., 1990. Society of Sports Therapists–a proposal. British Journal of Sports Medicine, 24(2), p.74.
- The Society of Sports Therapists. (Nd). What is Sports Therapy?. [Online]. The Society of Sports Therapists. Last Updated: Unknown. Available at: https://thesst.org/public-information/what-is-sports-therapy/ [Accessed 17 November 2023].
- Arif, H., Arif, F., Morales, J., Waldrop, I.W. and Sheets, N.W., 2023. Epidemiology of Rugby-Related Injuries Presenting to the Emergency Department: A 10-Year Review. Cureus, 15(6).
- Hoge, C., Sabbagh, R., Morgan, M. and Grawe, B.M., 2022. Epidemiology of youth and high school American football-related injuries presenting to United States emergency departments: 2010-2019. The Physician and sportsmedicine, 50(4), pp.332-337.
- Martin, C., 2001. The future for the field of sports medicine. British Journal of Sports Medicine, 35(4), pp.283-283.
- Waddington, I., Roderick, M. and Naik, R., 2001. Methods of appointment and qualifications of club doctors and physiotherapists in English professional football: some problems and issues. British journal of sports medicine, 35(1), pp.48-53.
- van Ierssel, J., Pennock, K.F., Sampson, M., Zemek, R. and Caron, J.G., 2022. Which psychosocial factors are associated with return to sport following concussion? A systematic review. Journal of sport and health science, 11(4), pp.438-449.
- Williams, S., Robertson, C., Starling, L., McKay, C., West, S., Brown, J. and Stokes, K., 2022. Injuries in elite men’s rugby union: an updated (2012–2020) meta-analysis of 11,620 match and training injuries. Sports medicine, pp.1-14.
Lenjani, B., Rahhiti, P., Shadbani, G., Demiri, A., Pelaj, B, Demi, A., Sylaj, R., Mulaj, E. V., and Lenjani, B. 2021. Emergency Medical Care and Mangement of Sports Injuries on the Football Court. Albanian Journal of Trauma and Emergency Surgery, 5 (1), pp. 773-777