Keywords: vertical jumps, testing, ACL, return to sport
Vertical jumps play a crucial role in the return-to-sport testing protocol following anterior cruciate ligament reconstruction (ACLR). This recommendation extends beyond athletes in jumping sports, as vertical jumps metrics are sensitive to detect lower limb deficits even without advanced equipment. However, the effectiveness of these tests relies heavily on how they are conducted and interpreted.
To translate research findings into clinical practice and to ensure consistent and valid results, here are 11 tips (figure 1) to ensure accurate and meaningful results from your jump testing sessions.
The clinical tips for vertical jumps testing are an extension of our recent study (1), published in the BJSM. The study utilizes four vertical jump tests—two bilateral and two unilateral—to monitor athletes’ progress.
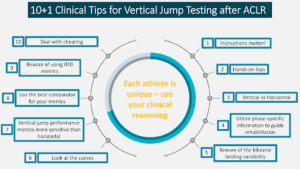
Figure 1. Summary of clinical tips for jump testing in athletes after anterior cruciate ligament reconstruction
Tip #1: Instructions matter!
Patients will change their strategy based on your instructions. Specify whether you want maximum height or speed during single-leg drop jumps to glean insights into knee and ankle joint performance. For the drop jumps we ask patients to jump as high and as fast as possible. They need to find their way in achieving both goals.
Tip #2: Hands on hips
Upper limb movement can contribute to jump performance therefore hands on hips ensure consistency within and between athletes. Have patients place their hands on their hips during vertical jump testing to ensure that the lower limbs are the primary contributors to the jumping motion.
Tip #3: Vertical vs Horizontal
Use vertical jumps to test concentric force generation ability and horizontal landing to test force absorption ability.2
Tip #4: Use bilateral vertical jumps to check for compensatory strategies
Bilateral jump tests provide valuable information about compensatory movement strategies between limbs. Identifying the phase (eccentric, concentric, final landing) that presents the greatest challenge in achieving symmetry is essential for targeted rehabilitation and training. Notably, during a countermovement jump, the concentric phase, particularly the second half timewise (the final push-off), proves to be the most demanding in terms of achieving bilateral symmetry.
Tip #5: Landing of vertical jumps
There is a significant variability in the peak landing force during bilateral jumps, with symmetry ranging from 50-150% in healthy athletes and athletes at the time to return to sport after ACLR. Athletes after ACLR initially avoid loading the injured leg but gradually reduce asymmetry as a result of increased confidence and capacity. Given an average asymmetry of 20% in healthy athletes, using a 90% symmetry cutoff may not be advisable.
Assessing symmetry in peak vertical landing force during unilateral vertical tasks may not offer meaningful or actionable information.
Tip #6: Look at the curves
Utilize force plates to examine force-time curves, providing phase-specific information and evaluating the stretch-shortening cycle function. Contact time is not enough to inform you about the strategy used to produce the performance reported.
Tip #7: Performance metrics
Vertical jumps performance metrics are very sensitive to monitor progress during rehabilitation. If you don’t have force plates you can measure performance metrics with great accuracy using phone applications.3
Tip #8: Choose your comparator
Carefully select the comparator for metrics, considering pre-injury data, normative data, or the uninvolved leg. Each option has strengths and weaknesses. While pre-injury data is the optimal choice, they are not always available. For double leg jumps ensure improvement over time and for single leg jumps target for symmetry between limbs if pre-injury data are not available.
Tip #9: Rate of Force Development (RFD)
Avoid using RFD metrics in the four tests mentioned, as the metric’s variability compromises the validity of RFD-related information. A recommended alternative is using a squat jump, instructing patients to jump with maximum speed and height to obtain more reliable data for evaluating force development.
Tip #10: Dealing with cheating
At the time to return athletes are “grand masters” in cheating, especially if they have been briefed on the test outcomes and key metrics. Eager to meet symmetry criteria, they employ various tactics like reducing performance during bilateral jumps to achieve better symmetry in the kinetics metrics or reducing performance of the uninvolved leg during the single leg jumps. To address this, it is advisable to obtain their maximum performance from previous tests as a baseline for comparison. Another way is to establish standardized thresholds and targets for unilateral Reactive Strength Index (RSI) during the drop jumps. Use impulse momentum instead of flight time for jump height calculation.
Tip #11: Every athlete is unique
Be careful when you use jump height and you compare your athlete’s performance to normative values. Jump height is influenced by factors like age, gender, and activity level. In the context of injury, the primary objective should be restoring symmetry, especially in the absence of pre-injury data, recognizing that each athlete is unique.
Based on research findings and our clinical experience we follow specific metrics for each test. These metrics are useful to get phase-specific information to guide rehabilitation after ACLR. For athletes with other injuries or healthy individuals there might be other or additional useful metrics.
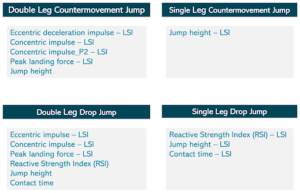
Figure 2. Key metrics during vertical jumps to monitor throughout rehabilitation and at the time to return to sport after anterior cruciate ligament (ACL) reconstruction.
Conclusion
Vertical jump testing should be an integral part of the periodic and return to sport assessment for athletes undergoing ACLR. However, it’s not just about conducting the test—it’s about selecting the right tests, adhering to relevant metrics, and understanding the purpose behind the testing.
Authors and Affiliations
Roula Kotsifaki, Vasileios Sideris, Enda King, Rod Whiteley
Rehabilitation Department, Aspetar, Orthopaedic and Sports Medicine Hospital, Doha, Qatar
Authors have no competing interests.
References
- Kotsifaki R, Sideris V, King E, Bahr R, Whiteley R. Performance and symmetry measures during vertical jump testing at return to sport after ACL reconstruction. Br J Sports Med. Oct 2023;57(20):1304-1310. doi:10.1136/bjsports-2022-106588
- Kotsifaki A, Van Rossom S, Whiteley R, et al. Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes. Br J Sports Med. May 2022;56(9):490-498. doi:10.1136/bjsports-2021-104692
- Whiteley I, Sideris V, Kotsifaki R, King E, Whiteley R. The MyJump App is a Valid Method of Assessing and Classifying Limb Symmetry During Recovery from Anterior Cruciate Ligament Reconstruction. Int J Sports Phys Ther. 2023;18(5):1156-1165. doi:10.26603/001c.88005