Authors: Lianne Wood, Stevie VanHegan, Janet Norris on behalf of the author team Sarah Dean, Nadine E Foster, Andrew Booth, Vicky Booth and Jill Hayden
In this blog we will explain the findings of a realist review to explore how therapeutic exercise prescription can be optimised for persistent non-specific low back pain. When we refer to therapeutic exercise prescription, we mean exercise prescribed by a health care professional for people with persistent low back pain, or low back pain that is non-specific and chronic, lasting over 3 months. Our study was funded by the Orthopaedic Research UK Charity.
Why is this study important?
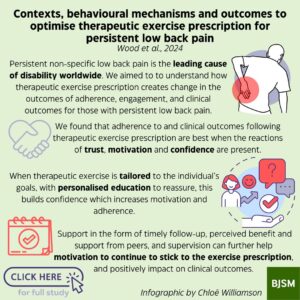
Persistent non-specific low back pain is the leading cause of disability worldwide. Although therapeutic exercise is widely recommended, the effects on pain and physical function are not much different to any other treatment for low back pain in the short or long term.
Therapeutic exercise (such as stretching, strengthening, aerobic exercise or specific exercise types like Pilates) has been proposed to reduce low back pain and improve function through various mechanisms or ‘reactions’. When we refer to a reaction, we mean how the exercise may work to create a change. It is unclear how these proposed reactions are triggered and under what conditions they are activated. Neither do we know if different reactions lead to different outcomes. The aim of this study therefore was to understand how therapeutic exercise prescription creates change in the outcomes of adherence, engagement, and clinical outcomes for those with persistent low back pain.
How did the study go about this?
We used a method called ‘realist evidence synthesis’. Realist methods aim to understand what works, for whom, in what contexts and why. Realist reviews develop initial programme theories about how the treatment may work, before testing and refining these theories.
We first developed initial programme theories, using literature reviews and having stakeholder group meetings. Stakeholders included patients, physiotherapists, personal trainers and a psychologist. An example theory is “When a person with persistent low back pain builds a positive therapeutic alliance, then they will be motivated to engage with the prescribed exercise”. Therapeutic alliance is how you and a therapist connect, behave and engage with each other.
We then used a further search to refine these programme theories, before testing them against further literature and in stakeholder groups. We analysed the richness, rigour and relevance of each study and used thematic analysis to extract data. We also assigned an overall confidence in the results. We included a total of 75 studies and worked with a total of 8 patient and clinician representatives to refine the programme theories.
What did the study find?
We found that the development and maintenance of (1) trust, (2) motivation and (3) confidence are the key reactions involved in therapeutic exercise prescription, bringing about changes in engagement, adherence and clinical outcomes for those with persistent low back pain. Trust appeared to underpin the therapeutic exercise prescription as a marker and measure of the therapeutic alliance, and was necessary for the development of confidence and motivation. A holistic assessment of the patient, development of rapport and therapeutic alliance, and consideration of the patient’s previous experiences was important to facilitate a trusting relationship. When trust was established, an individualized exercise prescription was more likely.
When exercise was prescribed in a way that was perceived to be beneficial, enjoyable, and tailored to the individual’s preferences (both in difficulty, setting and exercise type) this enhanced patient motivation. When clinicians provide tailored education and reassurance, supervision of exercises, timely follow-up, and peer support (when necessary), this facilitated patient confidence and motivation to engage and adhere to the exercise prescription. Further, clinician confidence (and credibility) can impact the amount and type of support provided, as well as the development of a trusting relationship, and the patient’s motivation through individualized prescription.
What are the key take-home points?
We found that adherence to and clinical outcomes following therapeutic exercise prescription are best when the reactions of trust, motivation and confidence are present.
The contextual features of therapeutic alliance and development of rapport are important foundations to the development of trust and facilitate holistic assessment in order to identify and plan individualised treatment. When therapeutic exercise is tailored to the individual’s goals, with personalised education to reassure, this builds confidence which increases motivation and adherence.
Support in the form of timely follow-up, perceived benefit and support from peers, and supervision can further help motivation to continue to stick to the exercise prescription, and positively impact on clinical outcomes.