Osteoporotic fractures may affect one woman in two and one man in five, potentially causing pain, disability, loss of independence and increased mortality. Exercise may benefit risk of osteoporotic fracture by increasing muscle and bone strength and reducing falls risk. However, many health professionals are unsure of what exercise to recommend and concerned about potential risks of fracture during exercise. Existing guidance leaves some questions unanswered. We thus aimed to agree on the optimum physical activity and exercise to optimise bone strength, reduce risk of falls and fractures, improve posture and manage vertebral fracture symptoms, whilst minimising potential risks in people with osteoporosis.
How was it conducted?
The consensus process involved consultation with people with osteoporosis , as well as an expert group of health professionals and researchers to refine the scope. It was informed by a literature review and recommendations were then made based on evidence, or where this was lacking, from expert consensus.
What did we find?
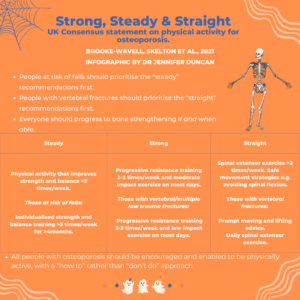
Guidance was provided in three main areas: exercise to improve bone strength (“strong”), to reduce falls risk (“steady”) and to increase spinal extensor strength to reduce risk of falls and vertebral fractures (“straight”).
Strong
To improve bone strength, we recommend strength training, combined with moderate impact exercise in those without vertebral or multiple low trauma fractures. The strength training would ideally be progressive resistance training, with guidance to establish safe technique. Once this is mastered, loads should gradually increase until they are heavy enough that the weight can only be lifted 8-12 times before needing to rest. The number of repetitions should progress to up to 3 sets of up to 8 repetitions, separated by rest pauses. Exercises should load major muscle groups, particularly focussing on spine and hip.
Moderate impact exercise may include activities such as low jumps, skipping, dancing or aerobics. People should aim to include 50 impacts (on each leg), separated by rest pauses, on most days. People with vertebral fracture or multiple low trauma fractures may instead do low impact exercise, such as walking or more gentle dancing, for 20 minutes per day.
Steady
In people at risk of falls, the primary recommendation is for strength and balance training, ideally individualised, delivered by a health or exercise professional and conducted for at least 3 hours per week over at least four months. This may be accessed by referral to a falls service. In those not eligible, twice weekly activities that improve strength and balance, such as Tai Chi, dance, yoga or Pilates may offer some benefit.
Straight
Everyone with osteoporosis would benefit from advice on safe lifting and moving strategies; ideally amending rather than prohibiting activities. Postural exercises (e.g. of spinal extensors) are recommended to benefit pain, kyphosis and vertebral fracture risk. For those with vertebral fractures, prompt advice from a physiotherapist is ideal to improve confidence to move safely.
Safety
Review of the literature showed very few fractures arising from exercise, although some cases were related to extreme, loaded or repetitive spinal flexion. For safety we thus recommended avoiding postures involving a high degree of spinal flexion and also that those with vertebral or multiple low trauma fractures should usually exercise only up to an impact equivalent to brisk walking.
Key points
People at risk of falls should prioritise the “steady” recommendations first and gradually progress to bone strengthening. Similarly, people with vertebral fractures should prioritise the “straight” recommendations first and progress to bone strengthening if and when able. Most importantly, all people with osteoporosis should be encouraged and enabled to be physically active, with a “how to” rather than “don’t do” approach.
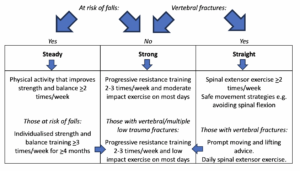
Flowchart of recommendations for bone strengthening.
Resources:
Resources to support the statement are available here: https://theros.org.uk/information-and-support/bone-health/exercise-for-bones/how-to-build-up-exercise-for-your-bone-strength/
The full consensus statement is available here: https://bjsm.bmj.com/content/bjsports/56/15/837.full.pdf
Consensus Statement Authors:
Katherine Brooke-Wavell 1*, Dawn A Skelton 2*, Karen L Barker 3, Emma M Clark 4, Sarah De Biase 5, Susanne Arnold 6, Zoe Paskins 7, Katie R Robinson 8, Rachel Lewis 9, Jonathan H Tobias 10, Kate A Ward 11, Julie Whitney 12, Sarah Leyland 13.
*joint first authors
Affiliations
1 Dr Katherine Brooke-Wavell, Senior Lecturer in Human Biology, National Centre for Sport and Exercise Medicine (East Midlands), School of Sport, Exercise and Health Sciences, Loughborough University;
2 Professor Dawn A Skelton, Professor in Ageing and Health, School of Health and Life Sciences, Glasgow Caledonian University;
3 Professor Karen L Barker, Professor of Physiotherapy, Physiotherapy Department, Nuffield Orthopaedic Centre, University of Oxford;
4 Prof Emma M Clark, Professor of Clinical Musculoskeletal Epidemiology, Bristol Medical School, University of Bristol, and Consultant Rheumatologist, North Bristol NHS Trust;
5 Sarah De Biase, AGILE Chair (Chartered Society of Physiotherapy recognised Professional Network for physiotherapists working with older people); Allied Health Professional Lead Older People’s Mental Health Service, Bradford District Care NHS Foundation Trust;
6 Dr Susanne Arnold, AGILE Secretary (Chartered Society of Physiotherapy recognised Professional Network for physiotherapists working with older people); Research Fellow, Warwick Clinical Trials Unit, University of Warwick;
7 Dr Zoe Paskins, Reader and Honorary Consultant in Rheumatology at the Primary Care Versus Arthritis Centre, Keele University;
8 Dr Katie R Robinson, Senior Research Fellow at the Academic Unit of Injury, Inflammation and Recovery Sciences, School of Medicine, University of Nottingham;
9 Rachel M Lewis, Clinical Specialist Physiotherapist in Rheumatology, North Bristol NHS Trust;
10 Professor Jonathan H Tobias, Professor in Rheumatology, Bristol Medical School, University of Bristol; Honorary Consultant North Bristol NHS Trust;
11 Professor Kate A Ward, Professor of Global Musculoskeletal Health, MRC Lifecourse Epidemiology Centre, University of Southampton;
12 Dr Julie Whitney, Lecturer in Long Term Conditions, Kings College Hospital, London; Consultant AHP, King’s College London
13 Sarah Leyland, Osteoporosis Nurse Consultant, Royal Osteoporosis Society, Bath.
X:
Katherine Brooke- Wavell @KBrookeWavell, Dawn A Skelton @LaterLifeTrain, Karen L Barker @ProfKarenB, Emma M Clark @emcbristol, Sarah De Biase @sarahdebiase, Susanne Arnold @AGILECSP, Zoe Paskins @zpaskins, Jonathan H Tobias @JonTobias1 and Kate A Ward @KateAWard17
Competing interests KB- W, KB; EMC, SDB, SA, ZP, KRR, RML, JHT, KAW, JW and SL have no competing interests to declare. DAS is a director of Later Life Training, a not- for- profit organisation that provides training and qualifications to health and fitness professionals working with frailer older people.
Funding Development of the statement was facilitated by funding by the Royal Osteoporosis Society, UK.