Is it an acute tear or wear & metabolic disrepair? A community MSK approach to managing the painful shoulder.
Key words: #MSKplaybook #Mindthesofttissuegap #rotatorcuff #tendinopathy #SEM #rotatorcufftear #subacromialimpingment
Introduction:
The rotator cuff muscles and tendons work as a dynamic structure to centralise the humeral head and aid movement, acting with the deltoid muscle and each other as force couples to keep the glenohumeral joint functioning and stable. The structural integrity and mechanical properties of the rotator cuff tendons are key to their function, with tears of the tendon and muscle degeneration being associated with pain and dysfunction. There is, however, an overlap between structural findings seen on both symptomatic (chronic tendon-related pain) and asymptomatic tendon tears. We discuss some of the current concepts around surgical repair, and whether the metabolic cascade of disrepair could explain chronic rotator cuff tendon pain associated with tears.

Figure 1: The MSK Playbook on rotator cuff tears
Tendons are not just a pulley, they are metabolically active and adaptable.
In the past, tendons were thought to be metabolically inert, but recent research has shown that although they have a relatively low metabolic rate (compared to muscle), they are capable of energy productions (glycolysis and mitochondrial respiration), with inflammatory signalling directly affecting tendon cell metabolism (1,2). Changes to their structure at a histological and macroscopic levels has been studied extensively, and changes in one or both of these predisposes patients to tendon tears of rotator cuff related pain (see Figure 2(3)). It is key to remember, that unlike muscles, tendons lack a blood supply, evident through their white substance; tears are more likely in tendons than muscles.
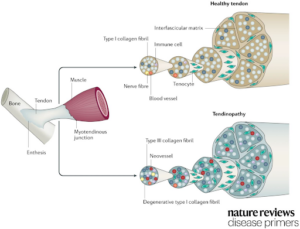
Figure 2: Structural changes in tendinopathy (4)
Type 1 collagen is the most abundant connective tissue in tendons, but these can degenerate over time, or in response to injury or due to metabolic conditions (e.g. diabetes (5)). This can affect a tendon’s properties leading to (6):
- A loss of tensile strength,
- A loss of shock absorption,
- Reduced tenocyte and tenoblast activity
- A loss of the ability to transmit force from muscle to joint movement.
- Increased sensitivity/pain due to innervation and blood supply of the covering epitenon
- An increased risk of tears
It is important to note that a tendon’s characteristics in terms of structure, shape and tensile strength vary by anatomical location and loading (stress). The response to injury of each tendon is therefore variable and a tailored “a la carte” approach should be used as part of a shared decision-making process during treatment.
The main treatment options for rotator cuff tendinopathy can be split into operative and non-operative treatment options. A recent multi-centre trial (CSAW) compared the effectiveness of non-surgical treatment (physiotherapy), to sham surgery and arthroscopic sub-acromial decompression and demonstrated that there was no significant difference in clinical outcomes between all three interventions (7). This is supported by further global evidence including randomised trials in the Cochrane Database (8).
| Non operative options | Operative options |
|
|
Evaluating a tendon tear; 5 features to consider
Evaluation of rotator cuff tendon tears should always be performed in the context of the patient’s function (guided by the clinical exam) and impact on the patient’s ADL’s, hobbies, and exercise goals. Rotator cuff tears can also overlap with other conditions, most commonly with frozen shoulder (adhesive capsulitis) in the same age group. Rotator cuff tears – may be painful, but do not produce the same capsular restriction to passive range of motion as frozen shoulder. There are 5 key features to be considered in evaluating a tendon tear (Figure 3)

Figure 3: AGASST system for grading tendon tears
The characteristics of tears can help determine the clinical management, with partial tendon tears of the articular side being 2-3 more likely than bursal side tears (9), and can usually be managed non-operatively. Full thickness tears, higher grade muscle atrophy (classified according to Goutallier classification, see Figure 4) and non-repairable tears are all associated with higher rates of tendon repair failure. The recent UKUFF trial demonstrated that repairable tears with evidence of healing had the best outcomes and tears that were not repairable at surgery were associated with the worst outcomes (18).
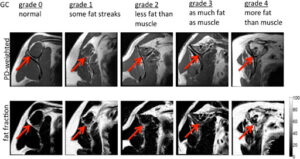
Figure 4: Goutallier classification (10)
Comparing imaging modalities: MRI or Ultrasound for tears?
Magnetic resonance imaging (MRI/MRA) (Figure 5) and ultrasound (US) are the preferred imaging modalities for imaging and evaluating tendon tears. When adequately trained to use and interpret each of these imaging modalities, it has been shown that there is no significant difference in their sensitivity for diagnosing full- and partial- thickness rotator cuff tears (11). The rate of (false positives) of tears reported on imaging (MRI) but not present on arthroscopy can increase with conditions such as adhesive capsulitis (12).
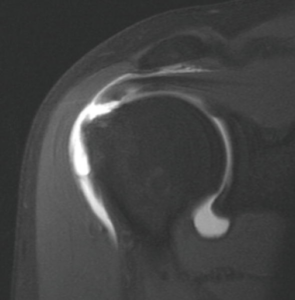
Figure 5: Magnetic resonance arthrogram T1 fat saturated, full thickness supraspinatus tendon tear shown in this coronal oblique image. Can see contrast leakage from joint capsule into sub-deltoid space (13).
In the clinic plain X-ray views can be useful to detect osteoarthritis and humeral migration. The present of a high riding humeral head (12,13) on AP radiographs points towards a probable diagnosis of a massive rotator cuff tear. It is important however to put imaging in the context of the patient’s pain and dysfunction, examples of this include:
- When a rotator cuff tear is seen alongside a frozen shoulder, treat the frozen shoulder first.
- Tendon abnormality does not always = pain, as evidence by the rate of asymptomatic tears (36)
Activity related shoulder pain and dysfunction has been commonly reported in the context of patients with normal sonographic appearance on US (14,36).

Figure 6: RCT management options
Once an acute rotator cuff tear is confirmed, urgent referral to a specialist surgeon is advised to discuss potential surgical management and repair. This will consider patient factors such as tear locations, the presence of fatty infiltration, the grade of the tear, the patient’s function and age (16).
Indications that support tendon repair:
- Tear due to high-energy traumatic injuries,
- Patients in a high-performing role that requires shoulder use for (sport/hobby),
- Younger patients (age < 50) or (age >50 with high function or demand of shoulder)
- Where non-operative management has failed, and after shared decision making where repair is deemed appropriate.
Time is a critical factor for acute repairs, with delay in presentation, tendon retraction, and muscle atrophy all associated with poor prognosis and outcomes from tendon repair (17).
| Example referral criteria for community MSK | |
| Non traumatic tears | Traumatic tears |
AND MRI/US/CT suggests:
|
Refer urgently for imaging and assessment if:
|
| *Risk factors such as smoking status, diabetes, and chronic MSK pain features should be included in the referral. | |

Figure 7: Community MSK approach to rotator cuff tears
Common tendon repair techniques
It is important to keep in mind the patient’s co-morbidities during management, since those with significant metabolic disrepair will have altered tendon structure (3), which may influence the cuff repair technique used.
There are three techniques:
- Traditional open repair – for large tears.
- Mini-open repair – both arthroscopic and via small incision.
- Arthroscopic repair.
Data has shown that there is no statistical difference in outcomes between open vs arthroscopic rotator cuff repair, with the rate of re-tear being high in both groups (14). One of the key considerations in both techniques is minimising injury to the deltoid which can be more difficult in fully open repair (19,20).
| The success of tendon repair has been shown to be influenced by tear location, size and fatty infiltration (24) | |
| Trans osseous | Trans tendon |
| -Is the most common technique, as it allows for anchoring of the tendon to bone (Figure 8).
-Radiologically, the double row repair has shown better outcome with potentially lower re-tear rates than single row (15), but functionally there is no statistically significant difference (16) |
-Can be used for an all-inside arthroscopic repair technique of PASTA (partial articular-sided supraspinatus tendon avulsion) lesions.
-This does not cause bunching of the bursal side has been shown to improve shoulder function (17) |
|
|

Figure 8: types of repairs going from left to right – single row, double row, double row bridging repair (18)
The use of rehabilitation is key in both the pre and post operative period, with the aim of restoring function, range of movement and strength. Deltoid retraining is advised and there is no significant difference between early (first day post-op to 4 weeks) and conservative (3 to 8 weeks post-op) in terms of ROM, function, and rate of re-tears (19). Post-operative rehabilitation protocols vary significantly with the use of passive exercises, active exercises and loading post operatively subject to variation (29).
Approaches to massive tears; new techniques and optimising function
Massive cuff tears or irreparable tears present a challenge for rehab, as the treatment options are newer and consensus on treatment options has not been reached.
| Tendon transfer | Ortho space balloon | Suprascapular nerve block |
| -Usually considered in younger patient’s
– Examples include, substituting posterior superior tears of supraspinatus and infraspinatus with the lower trapezius muscles and latissimus dorsi or substituting subscapularis with pec major. -It is not clear which is the best option for tendon transfer (20,21). |
-Can be inserted arthroscopically and the aim is to prevent superior humeral translation.
– Outcomes from a large RCT are reported to be similar to arthroscopic debridement (32) and so not supported by NICE in the UK unless as part of research trials. |
-Can be considered for pain relief in irreparable rotator cuff injury (22).
-If effective, the patients can be referred for radiofrequency ablation. |
The rotator cuff tendons: all for one and one for all!
The tendons of the rotator cuff (supraspinatus, infraspinatus, teres minor and subscapularis), all insert into the humeral head. Therefore, when considering injury to any one of these tendons, the assessment should be on function or disability associated with the rotator cuff as a unit. Recent studies have shown that when one rotator cuff has histological changes (supraspinatus, the most commonly torn rotator cuff muscle) there are associated changes in gene expression (mRNA) of other tendons (subscapularis) of the rotator cuff before any tears of macroscopic changes are seen (23). This has led to the theory of metabolic disrepair (1) with intrinsic risk factors such as obesity, diabetes, hypoxia, age and metabolic syndrome linked with increased risk of tendon tears.
Grey Hair: Rotator cuff tear
By far the biggest risk factors for rotator cuff tears is age, with tears more common (age>50) and shown to negatively influence healing after RCT repair (24). According to a surveillance study in primary care, population prevalence was 22.2% for having at least one full-thickness tear; 14.9% for 60-69 year olds, 25.9% in 70-79 year olds and 29% in 80-89 year olds – with age increasing alongside tear severity (25). The use of routine scanning for cuff tears in primary care or MSK interface services, remains debated with surveillance studies showing high rates of tears in older adults, but that they are more likely to be asymptomatic 66% compared to 34% symptomatic when found (26).
Make sure you have a plan before you scan!
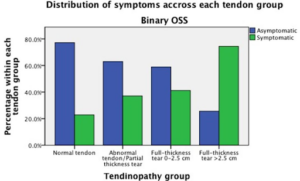
Figure 9: Distribution of symptoms across each tendon group (25)
In one primary care surveillance study, full thickness tears >2.5cm were associated with an increased ratio of symptomatic to asymptomatic tears (6), Other studies have also reported large-sized tears increased with age (26) and metabolic risk factors may be involved that impact tendon quality. As a result of chronical glenohumeral injuries and reduced loading activity with increasing age (23), the following are suspected to play a role in rotator cuff tendinopathy:
- Tissue senescence
- Tissue degeneration
- Altered mechanical stimuli
Prior to scanning, any RTC imaging should be placed in the context of the patient’s function, pain, and pre-test likelihood of finding a tear (age profile and existing medical conditions).
If you scan you will find.
One study of patients undergoing arthroscopic repair of symptomatic posterosuperior rotator cuff or subscapularis tear reported that 63.6% and 67.8% of patients had a tear of the opposite shoulder, respectively (on MRI) (27). These findings support the idea that tendon disrepair and underlying age or metabolic related factors could be driving atraumatic tears in the contralateral side in older adults. This needs to be considered in management, in terms of exercise therapy, orthopaedic management and injection options.
Non-operative management – physiotherapy
Non-operative management is generally first line for chronic, atraumatic RCTs, consisting primarily of:
- Physiotherapy
- Corticosteroid injections
- PRP (awaiting long-term high-quality evidence)
- NSAIDs
Physiotherapy involves manual therapy and exercise, focussing to ameliorate modifiable risk factors cuff such as the deltoid, pectoral muscles, glenohumeral internal rotation deficit (GIRD), weak stabilising, core muscles and weak and tight pelvic girdles (28). Since it helps prevent stiffness and strengthen the muscles, it is used as definitive treatment and post-operative rehabilitation. Exercise therapy is especially useful in the elderly population where surgery prognosis is poor (see Figure 10 (29, 30). However, no general consensus has been reached regarding the overall efficacy of exercise therapy (31) and its efficacy compared to that of surgery (32), due to the heterogeneity of outcome measures across randomised controlled trials and low-quality studies (such as not being specific to the size of tears studied). NICE guidelines recommend physiotherapy for postural correction, stretching and strengthening of the rotator cuff muscles and scapular muscles, manual therapy, and low-intensity high-frequency exercise based on pain threshold (33).
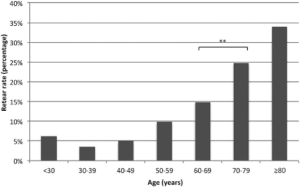
Figure 10: Rate of re-tears in age groups (29)
Non-operative management – injection therapy options, and chronic tendon related pain
Corticosteroid injection is an option for those with shoulder pain that is restricting rehab and has been shown to improve short term outcomes for (34):
- Improved pain
- Improved function
- Reduced insomnia at 8 weeks compared to no injection (35)
- Chance to develop deltoid function.
This must be balanced against the increased risk of tendon tears that some studies have reported (36). Some studies suggest that CSI use prior to surgery may result in adverse outcomes (37), whilst some suggest its use 4-6 weeks post-operatively may assist in rehabilitation and pain reduction (34). Recent studies have suggested that in chronic tendon related pain, other mechanisms such as neurogenic sensitisation (upregulation of nerve in growth factors & markers of neurogenic inflammation) could also explain chronic pain mechanism and may require alternate pain management options (38). Again, this shows the importance of treating the patient. For example, anxious/depressed patients are more likely to present with RCTs as they are more sensitive to pain (39).
Conclusions: are these mechanical fault lines in tendons or metabolic and age relate wear?
- Patient specific factors such as pain/function, rehab potential, mechanism of injury and duration of tear should be considered in treatment discussions.
- Shared decision making should focus on the patient’s level of function.
- The rotator cuff as a whole unit should be considered during rehab.
- Consider surgical and medical risk factors such as joint disease (OA), crystal arthropathies, chronic tendon related pain and metabolic conditions.
Authors and Affiliations: : Geethana Yogarajah, Irfan Ahmed, Niel Kang
Conceptualization: G.Y., I.A. and N.K.; Methodology: G.Y., I.A. and N.K.; Resources: G.Y., I.A. and N.K.; Supervision: I.A. and N.K.; Visualization: G.Y. and I.A.; Writing – original draft: G.Y.; Writing – review & editing: I.A. and N.K.;
Miss Geethana Yogarajah
5th year medical student, University of Cambridge
Dr Irfan Ahmed
Locum Consultant in Musculoskeletal, Sport & Exercise Medicine, Addenbrooke’s Hospital
Twitter @ExerciseIrfan
Mr Niel Kang
Consultant Trauma & Orthopaedic Surgeon
Cambridge University Hospitals NHS Trust
Affiliate Assistant Professor
Clinical school of medicine, University of Cambridge
Education and Careers Committee
British Orthopaedic Association
Twitter @kangstagram77
No relevant conflicts of interests or relevant disclosures declared by any of the authors.
Bibliography
- Ackerman, J. E., Best, K. T., Muscat, S. N. & Loiselle, A. E. Metabolic regulation of tendon inflammation and healing following injury. Curr. Rheumatol. Rep. 23, 15 (2021).
- Izumi, S., Otsuru, S., Adachi, N., Akabudike, N. & Enomoto-Iwamoto, M. Control of glucose metabolism is important in tenogenic differentiation of progenitors derived from human injured tendons. PLoS ONE 14, e0213912 (2019).
- Millar, N. L. et al. Inflammation is present in early human tendinopathy. Am. J. Sports Med. 38, 2085–2091 (2010).
- Millar, N. L. et al. Tendinopathy. Nat. Rev. Dis. Primer 7, 1–21 (2021).
- Leong, H. T. et al. Risk factors for rotator cuff tendinopathy: A systematic review and meta-analysis. J. Rehabil. Med. 51, 627–637 (2019).
- Abate, M. et al. Pathogenesis of tendinopathies: inflammation or degeneration? Arthritis Res. Ther. 11, 235 (2009).
- Beard, D. J. et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. The Lancet 391, 329–338 (2018).
- Lin, M.-T. et al. Comparative Effectiveness of Injection Therapies in Rotator Cuff Tendinopathy: A Systematic Review, Pairwise and Network Meta-analysis of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 100, 336-349.e15 (2019).
- Matava, M. J., Purcell, D. B. & Rudzki, J. R. Partial-Thickness Rotator Cuff Tears. Am. J. Sports Med. 33, 1405–1417 (2005).
- Nardo, L. et al. Quantitative assessment of fat infiltration in the rotator cuff muscles using water-fat MRI. J. Magn. Reson. Imaging 39, 1178–1185 (2014).
- Farooqi, A. S. et al. Diagnostic Accuracy of Ultrasonography for Rotator Cuff Tears: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 9, 23259671211035104 (2021).
- Loeffler, B. J., Brown, S. L., D’Alessandro, D. F., Fleischli, J. E. & Connor, P. M. Incidence of False Positive Rotator Cuff Pathology in MRIs of Patients with Adhesive Capsulitis. Orthopedics 34, 362 (2011).
- Lenza, M. et al. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst. Rev. 2013, CD009020 (2013).
- Carr, A. et al. Effectiveness of open and arthroscopic rotator cuff repair (UKUFF): a randomised controlled trial. Bone Jt. J. 99-B, 107–115 (2017).
- Franceschi, F. et al. Double-Row Repair Lowers the Retear Risk After Accelerated Rehabilitation. Am. J. Sports Med. 44, 948–956 (2016).
- Does Double-Row Rotator Cuff Repair Improve Functional Outcome of Patients Compared With Single-Row Technique? https://oce.ovid.com/article/00000475-201205000-00029.
- Itthipanichpong, T., Thamrongskulsiri, N., Limskul, D. & Tanpowpong, T. All-Inside Arthroscopic Partial Articular-Sided Supraspinatus Tendon Avulsion (PASTA) Repair Without Bunching of the Bursal Side of the Tendon. Arthrosc. Tech. 11, e1071–e1075 (2022).
- Rotator Cuff Injuries / Impingement Syndrome. Vasta Performance Training and Physical Therapy https://vastasports.com/physical-therapy/rotator-cuff-injuries-impingement-syndrome/.
- Mazuquin, B. F. et al. Effectiveness of early compared with conservative rehabilitation for patients having rotator cuff repair surgery: an overview of systematic reviews. Br. J. Sports Med. 52, 111–121 (2018).
- Osti, L. et al. Arthroscopic-assisted latissimus dorsi transfer for massive rotator cuff tear: a systematic review. Br. Med. Bull. 128, 23–35 (2018).
- Cartucho, A. Tendon transfers for massive rotator cuff tears. EFORT Open Rev. 7, 404–413 (2022).
- Agrawal, H., Pilania, C. & Gonnade, N. M. Suprascapular Nerve Block: A Technical Review. Indian J. Phys. Med. Rehabil. 33, 16 (2023).
- Plachel, F. et al. Risk Factors for Rotator Cuff Disease: An Experimental Study on Intact Human Subscapularis Tendons. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 38, 182–191 (2020).
- Rashid, M. S. et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop. 88, 606–611 (2017).
- Hinsley, H., Ganderton, C., Arden, N. K. & Carr, A. J. Prevalence of rotator cuff tendon tears and symptoms in a Chingford general population cohort, and the resultant impact on UK health services: a cross-sectional observational study. BMJ Open 12, e059175 (2022).
- Minagawa, H. et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J. Orthop. 10, 8–12 (2013).
- Yoon, T.-H., Kim, S.-J., Choi, Y.-R., Kang, K.-T. & Chun, Y.-M. Age, Tear Size, Extent of Retraction, and Fatty Infiltration Associated With a High Chance of a Similar Rotator Cuff Tear in the Contralateral Shoulder Regardless of Symptoms in Patients Undergoing Cuff Repair in the Index Shoulder. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. S0749-8063(23)00174–3 (2023) doi:10.1016/j.arthro.2023.02.008.
- Rodriguez-Santiago, B., Castillo, B., Baerga-Varela, L. & Micheo, W. F. Rehabilitation Management of Rotator Cuff Injuries in the Master Athlete. Curr. Sports Med. Rep. 18, 330 (2019).
- Diebold, G., Lam, P., Walton, J. & Murrell, G. A. C. Relationship Between Age and Rotator Cuff Retear: A Study of 1,600 Consecutive Rotator Cuff Repairs. JBJS 99, 1198 (2017).
- Harryman, D. T. 2nd et al. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. JBJS 73, 982 (1991).
- Ainsworth, R. & Lewis, J. S. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br. J. Sports Med. 41, 200–210 (2007).
- Longo, U. G. et al. Conservative versus surgical management for patients with rotator cuff tears: a systematic review and META-analysis. BMC Musculoskelet. Disord. 22, 50 (2021).
- Scenario: Rotator cuff disorders | Management | Shoulder pain | CKS | NICE. https://cks.nice.org.uk/topics/shoulder-pain/management/rotator-cuff-disorders/.
- Ha, J.-W., Kim, H. & Kim, S. H. Effects of steroid injection during rehabilitation after arthroscopic rotator cuff repair. Clin. Shoulder Elb. 24, 166–171 (2021).
- Buchbinder, R. & Haas, R. Optimising treatment for patients with rotator cuff disorders. The Lancet 398, 369–370 (2021).
- Lin, C.-Y. et al. A Positive Correlation between Steroid Injections and Cuff Tendon Tears: A Cohort Study Using a Clinical Database. Int. J. Environ. Res. Public. Health 19, 4520 (2022).
- Puzzitiello, R. N. et al. Adverse Impact of Corticosteroid Injection on Rotator Cuff Tendon Health and Repair: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 36, 1468–1475 (2020).
- Wasker, S. V. Z., Challoumas, D., Weng, W., Murrell, G. A. C. & Millar, N. L. Is neurogenic inflammation involved in tendinopathy? A systematic review. BMJ Open Sport Exerc. Med. 9, e001494 (2023).
- Park, J. H., Rhee, S.-M., Kim, H. S. & Oh, J. H. Effects of Anxiety and Depression Measured via the Hospital Anxiety and Depression Scale on Early Pain and Range of Motion After Rotator Cuff Repair. Am. J. Sports Med. 49, 314–320 (2021).