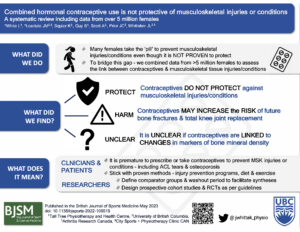
Many females use combined hormonal contraceptives (CHC) for non-contraceptive reasons, including to prevent musculoskeletal injuries (e.g., ACL tears, tendinopathy, fractures) and conditions (e.g.., osteoporosis, osteoarthritis) – even though they are not proven to be protective. To bridge this gap, we combined data from over 5 million females to assess the link between CHC use and various musculoskeletal conditions and injuries. This blog summarizes the full paper and explores why we did this, what we did and what we found (1).
Why is this study important?
Females are at higher risk of some sport-related musculoskeletal injuries like ACL tears and fractures compared to males. Females are also more likely to develop musculoskeletal conditions like osteoporosis and osteoarthritis (2) (3). Although this disparity is a result of both biological and socio-cultural factors, many females have been led to believe that their menstrual status is at fault (4). This has led some to use CHCs to stabilize the menstrual cycle. This practice is unproven. So, we conducted a systematic review, the highest form of evidence. They combine the findings of many studies into a single message that can be used to inform patients and healthcare providers.
What did we do?
Our systematic review only included studies designed (i.e., intervention and cohort studies) to assess the association between CHC use and the onset of any new musculoskeletal injury (e.g., ligament tears, tendinopathy, stress fractures) or condition (e.g., osteoporosis, osteoarthritis). We searched five databases for eligible studies. After assessing the risk of bias of included studies we performed a semi-quantitative synthesis to combine the findings for all musculoskeletal injuries or conditions (where ≥3 studies were available) to reach a conclusion about whether CHC use was beneficial or not.
What did the study find?
We found 50 studies, including over 5 million females, that were designed to assess the association between CHC use and musculoskeletal injuries or conditions. These 50 studies provided information about 30 different injuries or conditions but only 17 of the 30, had been investigated in ≥3 studies.
The findings can be summarized into three categories
- INSUFFICIENT INFORMATION ABOUT CHC USE: There were not enough studies (<3) that assessed the association of CHC use on ligament tears (including ACL tears), tendon ruptures, stress fractures or muscle strains to draw a conclusion about whether CHCs are protective or not.
- UNCLEAR INFORMATION ABOUT CHC USE: There was conflicting, low certainty evidence about most of the injuries and conditions where there were ≥3 studies. As a result, it is unclear if CHC use is protective for these injuries or conditions or not. As the evidence was of low certainty, it is likely that this conclusion will change as higher quality research studies become available.
- HARM WITH CHC USE: We found low-certainty evidence that CHC use is associated with small increases in risk of future fracture (any location, 20%) and total knee replacement (36%).
Although we did not find an association between CHC use and lumbar spine bone mineral density, a previous systematic review did find that adolescent CHC use may impair peak lumbar spine bone density accrual (5). These findings create an interesting link suggesting that CHC use early on in life may have some important long-term implications regarding future fracture risk.
What are the key take-home messages?
Despite identifying 50 studies, there is a lack of high-quality evidence about the relationship between CHC use and the onset of new musculoskeletal injuries and conditions.
What we can say, based on data from over 5 million females from around the globe, is that there is NO EVIDENCE that CHC’s protect against any musculoskeletal injury or condition including ACL tears. If anything, there is evidence that CHC use may in fact INCREASE the risk of future fractures and total knee joint replacement.
Based on these findings, it is premature to prescribe or pressure females to use CHCs to prevent musculoskeletal injuries or conditions particularly considering the fact that we already have other very effective methods such as injury prevention programs, diet, and exercise.
Authors:
Justin M. Losciale1,2
Lynita White3
Jackie L. Whittaker1,2
Affiliations:
1Department of Physical Therapy, Faculty of Medicine, University of British Columbia, Vancouver, Canada
2Arthritis Research Canada, Vancouver, Canada
3Tall Tree Physiotherapy and Health Centre, Vancouver, Canada
Twitter:
@JayLos18
@jwhittak_physio
ORCID:
Justin M. Losciale 0000-0001-5135-1191
Jackie L. Whittaker 0000-0002-6591-4976
References:
- White L, Losciale JM, Squier K, et alCombined hormonal contraceptive use is not protective against musculoskeletal conditions or injuries: a systematic review with data from 5 million femalesBritish Journal of Sports Medicine Published Online First: 24 May 2023. doi: 10.1136/bjsports-2022-10651
- Srikanth VK, Fryer JL, Zhai G, et al. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage 2005;13(9):769-81. doi: 10.1016/j.joca.2005.04.014
- Rollman GB, Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain 2001;17(1):20-4. doi: 10.1097/00002508-200103000-00004
- Herzberg SD, Motu’apuaka ML, Lambert W, et al. The Effect of Menstrual Cycle and Contraceptives on ACL Injuries and Laxity: A Systematic Review and Meta-analysis. Orthop J Sports Med 2017;5(7):2325967117718781. doi: 10.1177/2325967117718781 [published Online First: 2017/08/11]
- Goshtasebi A, Subotic Brajic T, Scholes D, et al. Adolescent use of combined hormonal contraception and peak bone mineral density accrual: A meta-analysis of international prospective controlled studies. Clin Endocrinol (Oxf) 2019;90(4):517-24. doi: 10.1111/cen.13932 [published Online First: 20190210]