
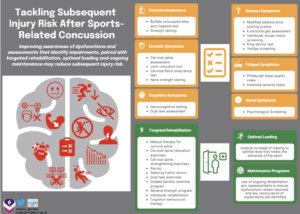
Active rehabilitation and graded exercise rather than physical rest may help reduce the increased injury risk reported in many recent studies.
Keywords: Sports-Related Concussion, Rehabilitation, Injury risk
Sports-Related Concussion (SRC) may increase subsequent injury risk (1–3), with disturbances to the neuromuscular control system often theorised as a contributing factor (4). Outside elite sport, protocols advise 14-days physical rest and 5-days graded Return To Play (RTP). Despite a link between high acute-on-chronic workload ratios and increased injury risk (5), little attention has been given to the effect of no physical exercise for 14 days and RTP shortly after this. This blog will go on to explore this further.
What may be causing the increased injury risk?
Neuromuscular control whilst performing complex tasks (often under fatigue) are qualities required for sporting activities. Impaired ability to perform these may increase injury risk (4),In particular, impaired neuromuscular control (6,7) has been associated with risk of cruciate ligament injury and deficient balance has been linked to ankle injury (8,9). Injury risk after SRC may be due to a variety of reasons:
- Altered balance: slow or inappropriate response to perturbations from impaired proprioception, motor control, Vestibular-Ocular-Motor (VOM) function and reduced strength (10–15).
- Poor movement patterns: altered processing of sensory feedback and feedforward mechanisms alter motor control, coordination, postural stability and agility (16,17).
- Slower reactions: altered integration and processing of stimuli and VOM dysfunction may alter anticipatory muscle activation and speed to react to others (18,19).
- Reduced strength: altered neural activity may reduce max strength and rate of force development, impairing movement efficiency (20,21).
- Neurocognitive function: reaction time and motor processing speed deficits may impair decision-making, affecting neuromotor (22–28) and sensorimotor control (1).
- Dual task activities: reduced physical and/or cognitive performance (29,30) may negatively affect physical performance whilst making strategic decisions.
- Physical loading tolerance: returning to too much load too quickly has been linked to increased injury risk (5).
Deficits have been reported up to 90 days post injury (11,31) and long after athletes have RTP (32,33). Despite these factors, many graded RTP protocols do not suggest focusing on any of the above aspects during or after RTP, this could leave athletes unable to cope with the demands of their sport.
How does this inform my practice?
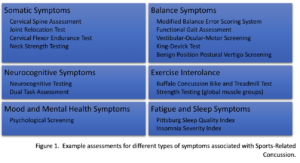
Extending SRC rehabilitation beyond the standardised protocols may reduce subsequent injury risk. Several assessments have been researched/studied, many detecting more than one dysfunction, and dysfunction of one system interacting and impairing function of another. For example, dysfunction of the cervical spine may produce, or contribute to, VOM dysfunction, consequently altering balance and coordination (34). Hence, clinicians should be aware treatment of a singular dysfunction may not resolve symptoms, and a multi-faceted approach to assessment and treatment is warranted (35–37). The Post-Concussion Symptom Scale may help clinicians to select which assessments are higher priority, depending on what type of symptoms are reported (Figure 1).
Using a symptom-based approach to assessment, clinicians can start a targeted approach to rehabilitation and monitoring after RTP, depending on what dysfunctions are present. For example;
- Vestibular and cervical rehabilitation has been shown to improve VOM dysfunction (34).
- Exercise intolerance can be treated with a graded increment of aerobic exercise (38).
- Dual task exercises may restore motor control, postural stability and ability to complete dual task activities (4).
- Strengthening neck and global muscle groups may reduce injury risk when returning to sport (39).
- Returning athletes to adequate loading prior to RTP will ensure the load is adequate to meet the demands of their sport.
Conclusion
- SRC increases subsequent injury risk through a variety of mechanisms.
- Motor control, spatial awareness, dual task activities, and reaction times may be affected long after athletes have RTP.
- A multi-faceted approach to assessment and rehabilitation during and following RTP may reduce injury risk.
Take home messages:
Authors and Affiliations
Kerry Glendona*, Glen Blenkinsopa, Antonio Bellib, and Matthew Paina
aSchool of Sport, Exercise and Health Sciences, Loughborough University, Loughborough, UK;
b Institute of Inflammation and Ageing, University of Birmingham, UK
*Physios in Sport Association: supports Chartered Physiotherapists who are interested in and or work in Sports & Exercise Medicine. Please follow this link to find out more information about their upcoming Golden Jubilee event on 1st July, which is open to all professions.
Authors have no competing interests.
References
- McPherson AL, Nagai T, Webster KE, Hewett TE. Musculoskeletal Injury Risk After Sport-Related Concussion: A Systematic Review and Meta-analysis. Am J Sports Med [Internet]. 2018 Aug 3 [cited 2019 Mar 19];1–8. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=30074832&site=ehost-live
- McCann R, Schussler E, Martinez J, Ramirez V, McCann R, Schussler E, et al. The Effect of Concussion History on Lower Extremity Injury Risk in College Athletes: A Systematic Review and Meta-Analysis. Int J Sports Phys Ther [Internet]. 2022 Aug 1;17(5):753–65. Available from: https://ijspt.scholasticahq.com/article/36810-the-effect-of-concussion-history-on-lower-extremity-injury-risk-in-college-athletes-a-systematic-review-and-meta-analysis
- Reneker JC, Babl R, Flowers MM. History of concussion and risk of subsequent injury in athletes and service members: A systematic review and meta-analysis. Musculoskelet Sci Pract [Internet]. 2019 Jul;42:173–85. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2468781218304260
- Avedesian JM, Singh H, Diekfuss JA, Myer GD, Grooms DR. Loss of Motor Stability After Sports-Related Concussion: Opportunities for Motor Learning Strategies to Reduce Musculoskeletal Injury Risk. Sport Med [Internet]. 2021 Nov 2;51(11):2299–309. Available from: https://link.springer.com/10.1007/s40279-021-01527-5
- Maupin D, Schram B, Canetti E, Orr R. The Relationship Between Acute: Chronic Workload Ratios and Injury Risk in Sports: A Systematic Review. Open access J Sport Med [Internet]. 2020;11:51–75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32158285
- Weiss K, Whatman C. Biomechanics Associated with Patellofemoral Pain and ACL Injuries in Sports. Sport Med [Internet]. 2015 Sep 1;45(9):1325–37. Available from: http://link.springer.com/10.1007/s40279-015-0353-4
- Swanik CB, Covassin T, Stearne DJ, Schatz P. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med [Internet]. 2007 Jun;35(6):943–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17369562
- McGuine TA, Greene JJ, Best T, Leverson G. Balance As a Predictor of Ankle Injuries in High School Basketball Players. Clin J Sport Med [Internet]. 2000 Oct;10(4):239–44. Available from: http://journals.lww.com/00042752-200010000-00003
- Trojian TH, McKeag DB. Single leg balance test to identify risk of ankle sprains. Br J Sports Med [Internet]. 2006 Jul;40(7):610–3. Available from: https://bjsm.bmj.com/lookup/doi/10.1136/bjsm.2005.024356
- HOWELL DR, OSTERNIG LR, CHOU L-S. Return to Activity after Concussion Affects Dual-Task Gait Balance Control Recovery. Med Sci Sport Exerc [Internet]. 2015 Apr;47(4):673–80. Available from: https://journals.lww.com/00005768-201504000-00001
- Catena RD, van Donkelaar P, Chou L-SS. Cognitive task effects on gait stability following concussion. Exp Brain Res [Internet]. 2007 Jan 7 [cited 2019 Mar 19];176(1):23–31. Available from: http://link.springer.com/10.1007/s00221-006-0596-2
- Parker TM, Osternig LR, Lee HJ, Van Donkelaar P, Chou LS. The effect of divided attention on gait stability following concussion. Clin Biomech. 2005 May;20(4):389–95.
- Parker TM, Osternig LR, Van Donkelaar P, Chou L-SS. Recovery of cognitive and dynamic motor function following concussion. Br J Sports Med [Internet]. 2007 Dec 1;41(12):868–73; discussion 873. Available from: http://bjsm.bmj.com/content/41/12/868.abstract
- Guskiewicz KM, Marshall SW, Bailes J, Mccrea M, Harding HP, MATTHEWS A, et al. Recurrent Concussion and Risk of Depression in Retired Professional Football Players. Med Sci Sport Exerc [Internet]. 2007 Jun [cited 2023 Apr 18];39(6):903–9. Available from: https://journals.lww.com/00005768-200706000-00002
- Matthews M, Johnston W, Bleakley CM, Davies RJ, Rankin AT, Webb M, et al. Concussion History and Balance Performance in Adolescent Rugby Union Players. Am J Sports Med [Internet]. 2021 Apr;49(5):1348–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33729858
- LYNALL RC, MAUNTEL TC, PADUA DA, MIHALIK JP. Acute Lower Extremity Injury Rates Increase after Concussion in College Athletes. Med Sci Sport Exerc [Internet]. 2015 Dec;47(12):2487–92. Available from: https://journals.lww.com/00005768-201512000-00001
- Harada GK, Rugg CM, Arshi A, Vail J, Hame SL. Multiple Concussions Increase Odds and Rate of Lower Extremity Injury in National Collegiate Athletic Association Athletes After Return to Play. Am J Sports Med [Internet]. 2019 Nov 12;47(13):3256–62. Available from: http://journals.sagepub.com/doi/10.1177/0363546519872502
- Clark JF, Ellis JK, Burns TM, Childress JM, Divine JG. Analysis of Central and Peripheral Vision Reaction Times in Patients With Postconcussion Visual Dysfunction. Clin J Sport Med [Internet]. 2017 Sep;27(5):457–61. Available from: https://journals.lww.com/00042752-201709000-00006
- Moore RD, Hillman CH, Broglio SP. The Persistent Influence of Concussive Injuries on Cognitive Control and Neuroelectric Function. J Athl Train [Internet]. 2014 Jan 1;49(1):24–35. Available from: https://meridian.allenpress.com/jat/article/49/1/24/112142/The-Persistent-Influence-of-Concussive-Injuries-on
- Reed N, Taha T, Monette G, Keightley M. A Preliminary Exploration of Concussion and Strength Performance in Youth Ice Hockey Players. Int J Sports Med [Internet]. 2016 Aug;37(9):708–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27191209
- Maffiuletti NA, Aagaard P, Blazevich AJ, Folland J, Tillin N, Duchateau J. Rate of force development: physiological and methodological considerations. Eur J Appl Physiol [Internet]. 2016 Jun 1 [cited 2023 Apr 24];116(6):1091. Available from: /pmc/articles/PMC4875063/
- Johnson EW, Kegel NE, Collins MW. Neuropsychological assessment of sport-related concussion. Clin Sports Med [Internet]. 2011 Jan;30(1):73–88, viii–ix. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21074083
- Tomás CC, Oliveira E, Sousa D, Uba-Chupel M, Furtado G, Rocha C, et al. Proceedings of the 3rd IPLeiria’s International Health Congress. BMC Health Serv Res [Internet]. 2016 Jul 6 [cited 2019 Mar 19];16(S3):200. Available from: http://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-016-1423-5
- Brooks MA, Peterson K, Biese K, Sanfilippo J, Heiderscheit BC, Bell DR. Concussion Increases Odds of Sustaining a Lower Extremity Musculoskeletal Injury after Return to Play among Collegiate Athletes. Am J Sports Med [Internet]. 2016 Mar 19 [cited 2019 Mar 19];44(3):742–7. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=s3h&AN=113451308&site=ehost-live
- Kardouni JR, Shing TL, McKinnon CJ, Scofield DE, Proctor SP. Risk for Lower Extremity Injury After Concussion: A Matched Cohort Study in Soldiers. J Orthop Sport Phys Ther [Internet]. 2018;48(7):533–40. Available from: https://www.jospt.org/doi/10.2519/jospt.2018.8053
- Herman DC, Jones D, Harrison A, Moser M, Tillman S, Farmer K, et al. Concussion May Increase the Risk of Subsequent Lower Extremity Musculoskeletal Injury in Collegiate Athletes. Sport Med [Internet]. 2017 May 20 [cited 2019 Mar 19];47(5):1003–10. Available from: http://link.springer.com/10.1007/s40279-016-0607-9
- Cross M, Kemp S, Smith A, Trewartha G, Stokes K. Professional Rugby Union players have a 60% greater risk of time loss injury after concussion: A 2-season prospective study of clinical outcomes. Br J Sports Med [Internet]. 2016 Aug [cited 2019 May 30];50(15):926–31. Available from: http://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2015-094982
- Pietrosimone B, Golightly YM, Mihalik JP, Guskiewicz KM. Concussion Frequency Associates with Musculoskeletal Injury in Retired NFL Players. Med Sci Sports Exerc [Internet]. 2015 Nov;47(11):2366–72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25871466
- Berkner J, Meehan WP 3rd, Master CL, Howell DR. Gait and Quiet-Stance Performance Among Adolescents After Concussion-Symptom Resolution. J Athl Train [Internet]. 2017 Dec 1 [cited 2019 Mar 19];52(12):1089–95. Available from: https://meridian.allenpress.com/jat/article/52/12/1089/112966/Gait-and-QuietStance-Performance-Among-Adolescents
- Parker TM, Osternig LR, VAN Donkelaar P, Chou L-S. Gait stability following concussion. Med Sci Sports Exerc [Internet]. 2006 Jun;38(6):1032–40. Available from: https://journals.lww.com/00005768-200606000-00002
- Catena RD, van Donkelaar P, Chou L-S. Altered balance control following concussion is better detected with an attention test during gait. Gait Posture [Internet]. 2007 Mar;25(3):406–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0966636206000981
- Cavanaugh JT, Guskiewicz KM, Giuliani C, Marshall S, Mercer V, Stergiou N. Detecting altered postural control after cerebral concussion in athletes with normal postural stability. Br J Sports Med [Internet]. 2005 Nov;39(11):805–11. Available from: https://bjsm.bmj.com/lookup/doi/10.1136/bjsm.2004.015909
- Meier TB, Lancaster MA, Mayer AR, Teague TK, Savitz J. Abnormalities in Functional Connectivity in Collegiate Football Athletes with and without a Concussion History: Implications and Role of Neuroactive Kynurenine Pathway Metabolites. J Neurotrauma [Internet]. 2017 Feb 15;34(4):824–37. Available from: http://www.liebertpub.com/doi/10.1089/neu.2016.4599
- Schneider KJ, Meeuwisse WH, Barlow KM, Emery CA. Cervicovestibular rehabilitation following sport-related concussion. Br J Sports Med [Internet]. 2018 Jan [cited 2020 Feb 4];52(2):100–1. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29127267
- Schneider KJ. Concussion – Part I: The need for a multifaceted assessment. Musculoskelet Sci Pract. 2019 Jul 1;42:140–50.
- Brown L, Camarinos J. The Role of Physical Therapy in Concussion Rehabilitation. Semin Pediatr Neurol. 2019 Jul 1;30:68–78.
- Schneider KJ. Concussion part II: Rehabilitation – The need for a multifaceted approach. Musculoskelet Sci Pract [Internet]. 2019 Jul 1 [cited 2020 Feb 4];42:151–61. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2468781219300177
- Leddy JJ, Hinds A, Sirica D, Willer B. The Role of Controlled Exercise in Concussion Management. Am Acad Phys Med Rehabil [Internet]. 2016 Mar [cited 2020 Feb 4];8(3):S91–100. Available from: http://dx.doi.org/10.1016/j.pmrj.2015.10.017
- Eckersley CP, Nightingale RW, Luck JF, Bass CR. The role of cervical muscles in mitigating concussion. J Sci Med Sport [Internet]. 2019 Jan 18 [cited 2019 Mar 19]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S1440244018309915