VIBE-MRI is a promising tool for the diagnosis of MSK injuries in radiation-sensitive athletes
Keywords: VIBE-MRI, musculoskeletal injuries, radiation exposure
Volumetric interpolated breath-hold examination (VIBE) is an MRI sequence that is increasingly being used by Sports and Exercise Medicine (SEM) clinicians, to evaluate sports injuries in radiation-sensitive populations (1). It offers the promise of evaluating osseous lesions and soft tissue injuries where time, patient comfort and early diagnoses are key to rehabilitation. This blog discusses how VIBE-MRI can be considered to help diagnose sports injuries in adult and adolescent athletes.
What makes VIBE-MRI different?
VIBE sequence MRI is a relatively new technique that was first developed in 1999. It has the benefit of being fast – producing high resolution images in under 30 seconds, when traditional sequences can take up to 30 minutes. Recently, it has been adapted for the diagnosis of MSK injuries, where reducing ionising radiation exposure and early diagnosis, can help to inform rehabilitation in young athletes.
| Modality | Typical effective doses (MsV) | Equivalent period of natural background radiation |
| CT Head | 2 | 1 year |
| CT Abdomen / Pelvis | 10 | 4.5 years |
| Lumbar X-Ray | 1.3 | 7 months |
| Limbs & Joints X-Ray (except hip) | <0.01 | <1.5 days |
| Hip X-Ray | 0.3 | 7 weeks |
| VIBE MRI | 0 | 0 |
Table 1: Radiation exposure of common MSK imaging modalities (2)
*2.2 MsV per year = Average natural background radiation in the United Kingdom
VIBE-MRI has the following additional benefits over standard MRI:
- High cortical resolution enables the identification of intracortical bone pathologies/fractures.
- Avoids the need of duplicate/additional scans, such as CT.
- Obtain high quality, multiplanar and 3D reconstruction images.
- Rapid scanning time – minimises discomfort in athletes with significant pain following an injury or those that have claustrophobia.
VIBE-MRI – Avoid the need for duplicate imaging.
- MRI scans have traditionally been more expensive than CT, however, the costs are decreasing.
- VIBE-MRI can also negate the need for duplicate imaging (MRI followed by CT). This is by providing soft tissue definition and images to detect fractures or osseous lesions in a single scan, where appropriate.
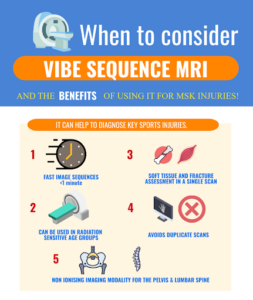
Figure 1: Infographic summarising VIBE-MRI
The following images show typical findings on Standard MRI Sequences:

Figure 2: Pars Fracture.
Sagittal T2 weighted image of the lumbar spine. Red arrow indicates a pars defect at L5/S1. There is also some grade 1 anterolisthesis.
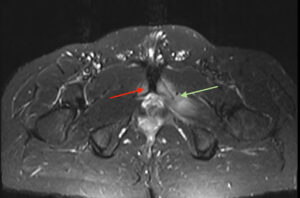
Figure 3: Osteitis Pubis
Axial STIR image of the pelvis. Red arrow shows the bone marrow oedema present at the pubic symphysis. Green arrow shows the adductor muscle oedema.
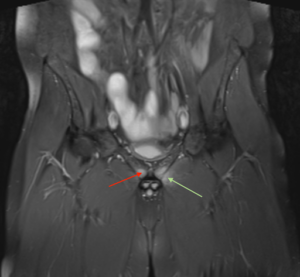
Figure 4: Osteitis Pubis
Coronal STIR image of the pelvis. Red arrow shows the bone marrow oedema present at the pubic symphysis. Green arrow shows the adductor muscle oedema.

Figure 5: Medial Tibial Stress Syndrome.
Axial STIR sequences of the tibia and fibula. There’s an increased fluid signal adjacent to the tibia, as shown by the red arrow. This scan shows a slightly atypical appearance, as the oedema is advancing to the posterior aspect of the tibia.
| Injury Type | Findings |
| Pars Fracture |
|
| Osteitis Pubis |
|
| Medial Tibial Stress Syndrome |
|
| Bankart Lesion |
|
Table 2: Typical findings on VIBE-MRI Sequences.
How does VIBE-MRI measure up to other imaging modalities?
In the world of elite sport and adolescent injuries, SEM clinicians are increasingly using VIBE-MRI to diagnose injuries. These sequences show good diagnostic accuracy for certain MSK injuries and can help provide key information to plan further interventions and rehabilitation.
| Injury | Standard MRI3 | VIBE-MRI4 | ||
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Pars Fracture | 81 | 99 | 97.7 | 92.3 |
| Injury | CT Arthrography5 | VIBE-MR Arthrography6 | ||
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Bankart Lesion | 89.4 | 96.4 | 95.7–100 | 93.9–97.0 |
| Glenoid Bone Loss | 100 | 100 | 95 | 93.8 |
| Injury | Ultrasound7 | VIBE-MR Arthrography8 | ||
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Rotator Cuff Tears
Full Thickness Partial Thickness |
91 68 |
93 94 |
55->92 |
92-94 |
| Injury | CT arthrography9 | VIBE-MRI9 | ||
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Elbow Loose Bodies
Anterior Posterior Either/Both |
64-91 92-100 88-100 |
33-67 54-69 20-70 |
46-91 92-100 88-100 |
13-73 15-77 20-60 |
Table 3: VIBE-MRI compared to other imaging modalities.

Figure 5: Infographic summarising when a VIBE MRI scan may be appropriate for sport-related injuries.
In conclusion, how can SEM clinicians utilise VIBE-MRI?
- VIBE-MRI produces fast sequence images, with good sensitivity for the detection of common sports-related, bone and soft tissue injuries.
- VIBE-MRI scans can help inform early diagnosis and management, reducing time lost to injury and enabling appropriate return to sport timelines.10 This is key for radiation-sensitive populations (adolescent and young adults).
- VIBE-MRI can prevent the need for dual scanning, using both CT and MRI, in complex soft tissue pathologies.
- Further studies are needed to evaluate the sensitivities and specificities of VIBE-MRI in a wider range of sports-related injuries. This could help to inform how and when VIBE-MRI scans can be used as the first line in injury management pathways.
Authors and Affiliations:
Mr Rifat Hassan, Dr Irfan Ahmed, Dr Haseeb Rehman, Dr Imran Lasker
No competing interest
No relevant disclosures
Rifat Hassan
Final Year Medical Student
University of Southampton
Twitter @RifatHassan_
Dr Irfan Ahmed
Sports and Exercise Medicine Consultant
Connect Health, United Kingdom
Twitter @Exerciseirfan
Dr Haseeb Rehman
Junior Doctor
York Hospital
Twitter @Haseeb2502
Dr Imran Lasker
Consultant Radiologist with Specialist interest in MSK
Employer: Mid and South Essex Foundation Trust
Twitter @DocLasker
Link to MSK/MRI courses: imranlasker.com, radiologyseminars.com. emergencyimaging.co.uk
References
- Koh E, Walton ERJ, Watson P. VIBE MRI: an alternative to CT in the imaging of sports-related osseous pathology? The British Journal of Radiology [Internet]. 2018 [cited 2022 Aug 4];91(1088). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6209485/
- Public Health England. Patient Dose information: guidance [Internet]. 2008 [cited 2022 Oct 22]. Available from: https://www.gov.uk/government/publications/medical-radiation-patient-doses/patient-dose-information-guidance
- Dhouib A, Tabard-Fougere A, Hanquinet S, Dayer R. Diagnostic accuracy of MR imaging for direct visualization of lumbar pars defect in children and young adults: a systematic review and meta-analysis. European Spine Journal [Internet]. 2018 May 1 [cited 2022 Sep 10];27(5):1058–66. Available from: https://link.springer.com/article/10.1007/s00586-017-5305-2
- Ang EC, Robertson AF, Malara FA, O’Shea T, Roebert JK, Schneider ME, et al. Diagnostic accuracy of 3-T magnetic resonance imaging with 3D T1 VIBE versus computer tomography in pars stress fracture of the lumbar spine. Skeletal radiology [Internet]. 2016 Nov 1 [cited 2022 Aug 4];45(11):1533–40. Available from: https://pubmed.ncbi.nlm.nih.gov/27614965/
- Khedr SA, Kassem HM, Azab MA. Comparative study of direct MR arthrography and CT arthrography with arthroscopic correlation in preoperative evaluation of anterior shoulder instability. Egyptian Journal of Radiology and Nuclear Medicine [Internet]. 2013 [cited 2022 Sep 11];44(4):817–27. Available from: https://www.sciencedirect.com/science/article/pii/S0378603X13000831?via%3Dihub
- Tian CY, Shang Y, Zheng ZZ. Glenoid bone lesions: Comparison between 3D VIBE images in MR arthrography and nonarthrographic MSCT. Journal of Magnetic Resonance Imaging [Internet]. 2012 Jul 1 [cited 2022 Sep 11];36(1):231–6. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/jmri.23622
- Roy JS, BraÃn C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: A systematic review and meta-analysis [Internet]. Vol. 49, British Journal of Sports Medicine. 2015. p. 1316–28. Available from: http://dx.doi.org/10.1136/bjsports-2014-094148
- Vandevenne JE, Vanhoenacker F, John JMM, Gelin G, Parizel PM. Fast MR arthrography using VIBE sequences to evaluate the rotator cuff. Skeletal Radiology [Internet]. 2009 Jul 18 [cited 2022 Aug 7];38(7):669–74. Available from: https://link.springer.com/article/10.1007/s00256-009-0677-y
- Dubberley JH, Faber KJ, Patterson SD, Garvin G, Bennett J, Romano W, et al. The detection of loose bodies in the elbow. The value of MRI and CT arthrography. Journal of Bone and Joint Surgery – Series B [Internet]. 2005 [cited 2022 Aug 24];87(5):684–6. Available from: https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.87B5.14851
- Beech M, Nagra NS, Wedatilake T, Kluzek S. Symptomatic stress reaction of the humerus in a professional cricketer. BMJ Case Reports [Internet]. 2019 Sep 1 [cited 2022 Aug 4];12(9):e227088. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6754635/