Love of basketball drove me to become a sports medicine doctoral student
From the moment I started playing basketball, I was obsessed. I spent days, months, and years learning the game of basketball and sweating on the basketball court. Sometimes, I would imagine myself as Jeremy Lin on the court at Madison Square Garden.
After leaving high school, I came to Fudan University Shanghai Medical College, where I majored in clinical medicine and played for the college’s basketball team as the captain. Seeing a lot of sports injuries on the basketball court made me rethink the relationship between sports and medicine. I realized I wanted to learn more and chose sports medicine as my future career.
In 2019, I began my doctoral study in Sports Medicine at Huashan Hospital affiliated with Fudan University. I am now in the third year of my Ph.D., engaging in research of skeletal muscle injury and rotator cuff tear under the supervision of my mentors.
The rupture occurred at the beginning of my career in sports medicine
On September 22, 2019, in my first basketball game as a graduate student, I felt in good physical condition and performed well in the first half. However, due to a lighting failure in the gymnasium, the halftime was too long, nearly an hour. At the beginning of the second half, I did a crossover, with the knee slightly bent. All of a sudden, I felt that my knee joint was “displaced” and then “reset” in an instant. That moment was like a buzzer beater in the game—the ball was flicked out of your fingertips, time seemed to stop, and you could hear your heart beating. Then with a muffled “bang” of the knee joint, the surroundings became noisy, and I fell to the ground uncontrollably.
After the rupture
My mentor, Dr. Jiwu Chen, an expert in sports medicine, contacted me when he heard about this. He gave me some practical suggestions, including wearing a knee brace immediately and using crutches to avoid secondary injuries.
On the night of the injury, the pain was not severe. I immediately iced the knee, wore a knee pad, and raised the injured leg with a pillow to reduce swelling before going to bed. The morning after the injury, the pain was severe. My injured knee was extremely swollen, filled with fluid, and unable to bend or straighten. I wore a knee brace and used crutches to avoid weight bearing on my injured knee.
This injury changed my role from a doctor to a patient. I used to tell patients to take a good rest. However, life after injury was not easy, such as hand numbness caused by holding crutches, difficulties in the shower or going to the toilet, etc.
Based on my professional knowledge, I thought the anterior cruciate ligament (ACL) might tear in the injured knee; but still expected an exception before the MR examination. An MRI scan taken at the 6th day after injury indicated that the ACL was torn, but luckily the meniscus was intact. Dr. Jiwu Chen performed a physical examination for me and confirmed that the stability my injured knee was good with negative Lachman test, anterior drawer test, and pivot-shift test.
Early ACL reconstruction or conservative treatment?
I read a lot about acute ACL injury and learned that current treatment options were still controversial. There were articles reporting that results did not differ between rehabilitation plus early ACL reconstruction versus rehabilitation plus optional delayed ACL reconstruction1. Considering my busy academic schedule and good joint stability, I decided to take the conservative treatment route.
Early rehabilitation is particularly important in conservative treatment. Dr. Jiwu Chen and the sports medicine team of Huashan Hospital customized a detailed rehabilitation protocol for me, which focused on pain/inflammation control, ROM, strength, and ultimately return to play.
Thirty-three days after injury, I was able to get back on the basketball court shooting with a heavy knee brace. Compared with the distorted and broken fibers in the MRI of the 6th day, the MRI demonstrated that the intensity signal of the ACL was much improved with fibers in continuity at the thirty-five days after injury. Probably, the ACL was partially torn actually, and the residual continuous fibers could not be shown because of the edema in the acute inflammation phase.

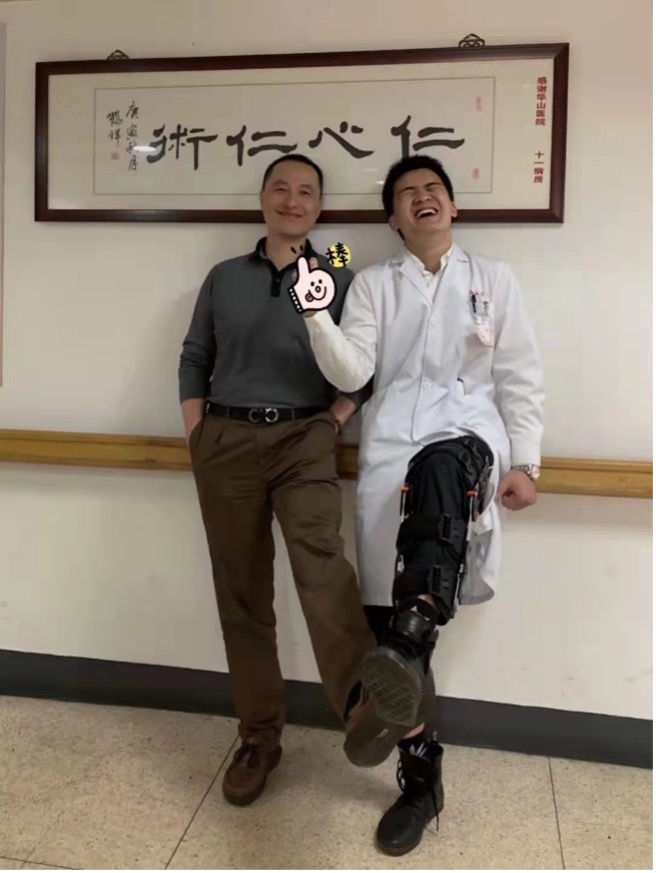
Through progressive and supervised rehabilitation, I managed to progress to 90° sidestep cutting maneuvers at 66 days, returned to training at 150 days, and returned to playing basketball at 200 days post injury. One year after the injury, I gradually returned to optimal performance and won the championship of Men’s Basketball Cup of Fudan University. Now my knee is functioning well and the ACL looks normal on MRI. But I do have occasional mild pain in my knee, and a certain level of psychological block.
TAKE HOME POINTS
In the past three years, two of my teammates also suffered ACL rupture. Because of my lucky story, they also chose conservative treatment. However, both of them failed, sprained again, and underwent ACL reconstruction surgery. One of them did not comply with the doctor’s instructions and returned to sports prematurely; the other had an ACL rupture with a torn meniscus and was overweight. These two cases made me think a lot.
In my opinion as a patient and as doctor, whether this case can be replicated depends on three elements:
- Good joint stability and MRI re-examination confirmed a partial ACL tear without other damage (i.e., meniscal tear);
- Early intervention of professional rehabilitation team;
- The patient’s good compliance with the doctor.
My case also raises questions about the timing of ACL reconstruction. The accuracy of MRI to distinguish complete from partial ACL tear when performed shortly after acute injury remains to be tested. Many doctors may recommend that surgery should be performed as soon as possible after a clear diagnosis of complete ACL tear by MRI. However, my case suggests that, through standard conservative treatment, supervised rehabilitation, and MRI re-examination, some patients can return to sports successfully. This question deserves more consideration for future research.
I realize my good outcome may be related to only a partial ACL tear, the absence of other damage, and early rehabilitation. I do feel that the full effect of my conservative treatment still needs to be tested over time to see if problems arise in the future.
Author and Affiliation:
Jinrong Lin
Department of Sports Medicine, Huashan Hospital, Fudan University, Shanghai, China.
Jrlin1996@gmail.com
Acknowledgements I would like to particularly thank Professor Jiwu Chen (Department of Sports Medicine, Shanghai General Hospital, Shanghai Jiao Tong University, Shanghai, China) and Professor Shiyi Chen (Department of Sports Medicine, Huashan Hospital, Fudan University, Shanghai, China) who helped me to write this article. The sports medicine team (Department of Sports Medicine, Huashan Hospital, Fudan University) for their medical advice and patience and my physiotherapist Longbing Wang (Tichuang Sports Center, Shanghai, China) for all the hours of rehabilitation spent together. Finally, the support from my family, friends, Shanghai Medical College basketball team and Huashan Hospital basketball team.
Competing interests None declared.
Ethics approval This study involves human participants but was not approved by an ethics committee or institutional board. This study is my own reflections on my own experiences and so an ethics approval was not undertaken. Participants gave informed consent to participate in the study before taking part.
Reference
- Frobell RB, Roos HP, Roos EM, et al. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br J Sports Med 2015;49(10):700. doi: 10.1136/bjsports-2014-f232rep [published Online First: 2015/05/01]