Return-to-running following childbirth: When the principles of Sports Medicine and Pelvic Health collide
In 2019 a BJSM blog highlighted the pelvic health considerations for return-to-running following childbirth and called for postpartum rehabilitation to align with return-to-sport injury models (Donnelly et al., 2019). We decided to answer its call for female-specific research and we wanted to provide new insights into how to evaluate and support perinatal women in order to facilitate their engagement in postpartum exercise, such as running.
What did we do and find?
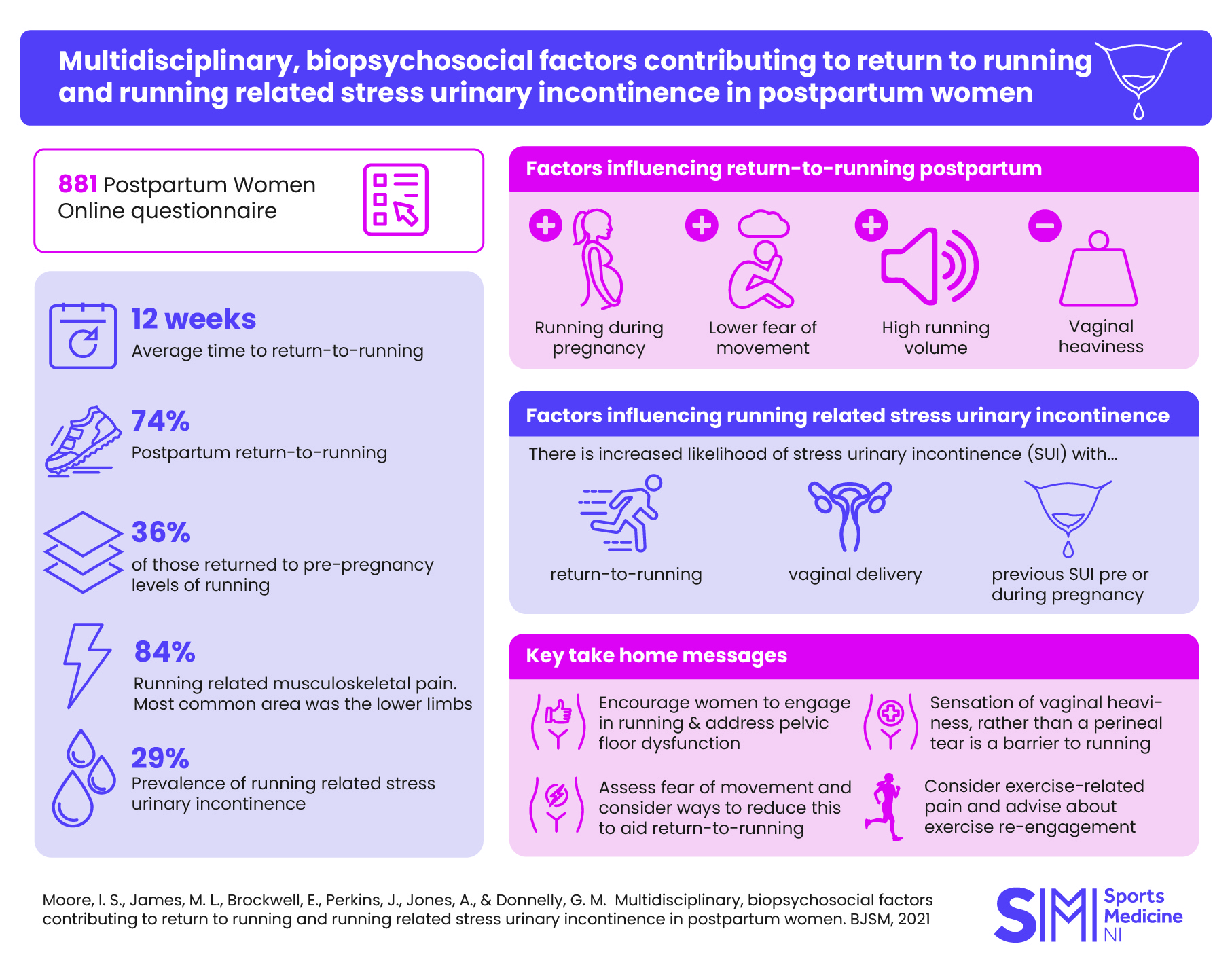
We designed an online survey exploring factors that may impact return-to-running postpartum (Moore et al., 2021). A large number of women (n=881) completed the survey and their average time to return-to-running postpartum was 12 weeks, which aligns with current clinical guidelines (Donnelly et al., 2020). The majority of women had returned to running (74%), however a high proportion (84%) suffered musculoskeletal pain whilst running. Pain in the lower limb was the most common complaint and likely related to this cohort being runners. Typically, lower back and pelvic pain are common issues postpartum, but these were less frequently reported than the lower limb in our study. We also identified modifiable and unmodifiable factors that contributed to postpartum return-to-running and running-related stress urinary incontinence (Figure 1).
Key factors for return-to-running (Figure 1 from Moore et al., 2021):
- Having lower fear of movement
- Engaging in running during pregnancy
- Running higher weekly volumes pre-pregnancy
- No sensation of vaginal heaviness
Key factors for experiencing running-related stress urinary incontinence (Figure 3 from Moore et al., 2021):
- Having returned to running
- A vaginal delivery
- Experiencing running-related stress urinary incontinence pre and during pregnancy.
What are the clinical ramifications?
For the first time, return-to-running postpartum was placed within a fear avoidance model. We identified that a low fear of movement increased the odds of return-to-running, which is similar to its impact on return-to-sport following an anterior cruciate ligament reconstruction. Therefore, clinicians should consider postpartum recovery and graded return-to-running with similar clinical reasoning to that which is currently used in return-to-sport. In particular, fear of movement should be addressed if required.
Importantly, women should be supported and empowered to continue running during pregnancy, where safe to do so. This not only offers important health benefits during pregnancy, but also increases the odds of return-to-running postpartum, enabling women to continue active lifestyles into motherhood.
Leaking urine whilst running occurred in one third of our cohort, but did not stop women running. We need to dispel the myth that incontinence is normal following childbirth; it may be common, but is not something women should have to live with. Regardless of whether women have returned to running postpartum, clinicians should screen for symptoms of pelvic floor dysfunction such as vaginal heaviness or leaking urine. If symptoms are present, this may indicate that the pelvic floor is not tolerating the high impact load involved. Similar to load tolerance evaluation in sports medicine (Gabbett, 2019), symptomatic women may need to regress the exercise load and modify activities until strength and conditioning needs are met.
Take-home messages: How to support postpartum return-to-running?
In keeping with sports medicine rehabilitation, perinatal services need to be proactive rather than reactive. Let’s stop assuming childbirth is a natural process only requiring natural recovery. Women experience significant physical and psychological changes during pregnancy and childbirth. The principles of rehabilitation encourage us to optimise recovery in any situation where function and wellbeing is compromised. If a sportsperson experiences trauma, rehabilitation needs are evaluated to optimise their recovery. Let’s honour women with the same values, principles and standards of care and ensure that equitable services are available across all populations.
Based on our findings we recommend the following when supporting perinatal women:
- Encourage continued engagement with running during pregnancy (where safe)
- Assess fear of movement following childbirth
- Screen for pelvic floor dysfunction (e.g., vaginal heaviness and leaking)
- Dispel the myth that leaking urine is normal
- Consider exercise-related pain
Written by Isabel S. Moore1, Megan L. James1, Alex Jones2 and Gráinne M. Donnelly3,4,5 on behalf of all the co-authors.
1Cardiff School of Sport & Health Sciences, Cardiff Metropolitan University, Cardiff, UK
2Department of Psychology, Swansea University, Swansea, UK
3Perinatal Physical Activity Research Group, Canterbury Christchurch University, Canterbury, UK
4Private practice, ABSOLUTE.PHYSIO, Maguiresbridge, UK
5University of Ulster, Coleraine, UK
Conflicts of interest: ISM is an Associate Editor for the British Journal of Sports Medicine
References
Donnelly, G., Brockwell, E., & Goom, T. (2019). Ready, steady…GO! Ensuring postnatal women are run-ready! Br J Sports Med. Retrieved 4th August 2021 from https://blogs.bmj.com/bjsm/2019/05/20/ready-steadygo-ensuring-postnatal-women-are-run-ready/
Donnelly, G. M., Rankin, A., Mills, H., De Vivo, M., Goom, T. S. H., & Brockwell, E. (2020). Infographic. Guidance for medical, health and fitness professionals to support women in returning to running postnatally. British Journal of Sports Medicine, 54(18), 1114. https://doi.org/10.1136/bjsports-2020-102139
Gabbett, T. J. (2019). How Much? How Fast? How Soon? Three Simple Concepts for Progressing Training Loads to Minimize Injury Risk and Enhance Performance. Journal of Orthopaedic & Sports Physical Therapy, 50(10), 570-573. https://doi.org/10.2519/jospt.2020.9256
Moore, I. S., James, M. L., Brockwell, E., Perkins, J., Jones, A., & Donnelly, G. M. (2021). Multidisciplinary, biopsychosocial factors contributing to return-to-running and running-related stress urinary incontinence in postpartum females. British Journal of Sports Medicine. https://doi.org/10.1136/bjsports-2021-104168