Muscle injury is the most common type of injury in athletes, especially in football players (Ekstrand (2011), Elliott (2011)). For this pathology, magnetic resonance imaging (MRI) is included in the diagnostic algorithm in most cases. To reach an adequate diagnosis and to obtain the best possible prediction of the RTP it is essential to work in multidisciplinary teams made up of sports doctors, orthopaedic surgeons, radiologists and physiotherapists. To make the interpretation of magnetic resonance images a little easier for each of the components of this team, we have decided to make this initial guide.
Standard MR protocol
In a standard MRI study, the behaviour of hydrogen protons when emitting a radio frequency pulse that excites them is assessed. Depending on the sequence being obtained (T1, T2, STIR …) we will assess the relaxation of the excited protons in different ways, or we will measure the amount of hydrogen protons that are present in the studied tissue (proton density (PD) weighted). To be able to emit the radio frequency pulse and to be able to hear the behaviour of the hydrogen protons, we need the coils that surround the region to be studied.
MRI is characterized by high soft tissue contrast, but we don’t just need contrast. As we already know, in order to assess the injured histoarchitecture (Balius 2020, Peña-Amaro 2021), we need images with high spatial resolution, which we will only achieve with high-field MRI equipment (3T or 1.5T equipment with powerful gradients).
The sequences used in standard muscle MRI protocols are divided into fluid-sensitive sequences (TSE T2 weighted or PD weighted with fat saturation) and anatomical sequences (T1 weighted). The first ones help to see if there is an acute muscle injury and analyze which part of the muscle histoarchitecture is injured (Balius 2020, Peña-Amaro 2021), and the latter allow to assess blood collections, scars that may be involved in the studied injury, and confirm the suspicion of artifacts in the first sequences (Isern-Kebschull 2020, Flores 2018, Guermazi 2017, Lee 2012).
The exploration is carried out by sections in the three planes of the space (axial, coronal and sagittal) and oblique planes following the direction of the injured myotendinous junction (MTJ). In some imaging protocols, water diffusion sequences and gradient echo sequences are added, but they are not part of the most commonly used sequences in general.
Muscle MRI
In the MRI of muscle, we will not only find connective tissue and muscle fibres. As we all know, there are more structures involved (adipose tissue, vessels, nerves, bones …), which can produce misunderstandings in the interpretation due to not knowing their normal appearance in MRI.
In liquid-sensitive sequences (T2 weighted or PD weighted with fat saturation) (Fig. 1), structures with a greater number of hydrogen protons and that at the same time these protons are more separated or free, will present more signal, that is, the image will be “whiter” (hyperintense). If we apply a descriptive and simple colour code it would be:
- Is the free fluid, intravascular fluid (vascular structures in longitudinal section) or joint fluid?
- White with a slight grey component: Extracellular matrix with higher water content (interstitial oedema), granulation tissue of the connective tissue in the immature healing phase. If the grey component is in the center of the structure it is a vessel (red circle).
- Grey: Corresponds to muscle fibres.
- Darker grey: It corresponds to saturated fat (bone marrow, intermuscular fat planes and subcutaneous fat tissue).
- Grey with black dots: Nerve (the nerve presents fatty tissue in the space between the nerve fascicles, between the perineurium) (Chen Y, 2019). Black dots would be the fascicles and the grey component the saturated fat tissue).
- Black: Cortical bone or connective tissue, fibrous scar.
- Heterogeneous black: Vascular structures in axial section.
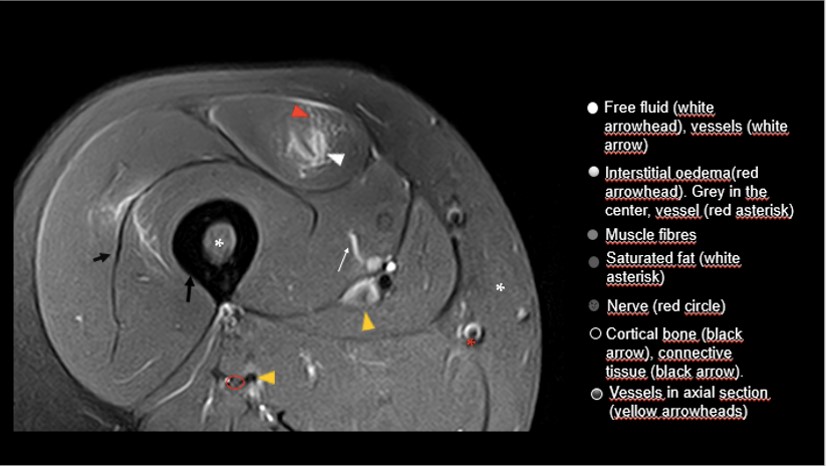
The behaviour of the vascular structures depends on the speed and morphology of the flow, in addition to various technical characteristics of the sequences. Sometimes in axial section we can see them with hypersignal (white with black spots), especially in the case of the veins. The morphology can help when we are dealing with an artery or a vein, the arteries have a muscular layer in their wall, and they are more round while the veins adapt to the adjacent structures and usually have more varied and oval morphologies.
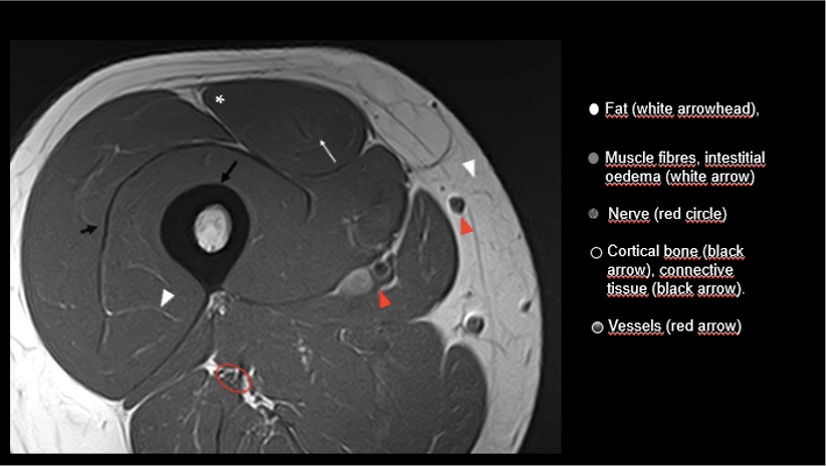
In T1 weighted (T1W) sequences (Fig. 2), the structures with a greater number of protons but highly clustered show a very short longitudinal relaxation time, and therefore are structures with more T1 signal, “whiter” (hyperintense). If we apply a descriptive colour code as we did before it would be:
- It corresponds to the fat that we can find in the bone marrow, in the subcutaneous fat, adjacent to the perimysium between the muscle fibres or perivascular between the muscle fibres.
- Muscle fibre, extracellular matrix with oedema, granulation tissue of the connective tissue in the immature healing phase.
- Grey with white dots. Nerve.
- Heterogeneous black / grey. In this case correspond to vascular structures.
- Connective tissue, cortical bone or fibrous scar.
We have indicated that both in the liquid-sensitive sequences and in T1W sequences the connective tissue is hypointense (black). The morphology of this connective tissue varies according to its distribution. As we already know, tendons in their origin or bone insertion show a more elongated morphology in the axial section (U or C shape), when they move away from their osteotendinous junction, they tend to be cordonal. When the muscle fibres anchor following the pennation angle, the connective tissue is distributed throughout the extracellular matrix (Balius 2020, Peña-Amaro 2021) and becomes thinner, spreading transversely through the muscular periphery and through intramuscular expansions.
Therefore, we will name as tendon the connective tissue in its cordonal section or with a thickness greater than a millimetre. When we find a millimetric connective tissue forming a sheet we will call it aponeurosis. Finally, when it becomes undetectable by MRI since it intermingles in the great network of the extracellular matrix, we will call it fascia.
Once we’ve understood how the different anatomical structures look like on the normal image, let’s quickly review the radiological signs of muscle injury. What characterizes the image of the muscle injury is the blood component that is distributed through different anatomical spaces. This component is free liquid, and therefore, we will see T2 / PD hypersignal (white) in the “gap” of a tendon structure, in the interstitial space between the muscle fibres (feather pattern), in the intermuscular space or in the gap that occurs when there is a rupture that affects muscle fibres. All these signs present an isointense signal with respect to the muscle on T1W sequences (grey).
If the injury does not involve a gap in muscle or tendon fibres, but rather a lesser degree of muscle rupture, we can find muscle fibres with a slight alteration of the MRI signal in the liquid-sensitive sequences (white with a slight grey component) without any representation in the T1W sequences. And in the case that the injury is severe, we will not only find an alteration of the MRI signal, but we will also find a morphological alteration of the MTJ consisting in connective tissue loss of tension and loss of the pennation angle, signs that we must assess in the coronal and sagittal planes.
When we study muscular injuries in hyperacute moments (less than 24 hours after the lesion), it is common to find practically no oedema, and this is when a vascular structure in longitudinal section can be confused with a focus of interstitial oedema in the liquid-sensitive sequence. The way to confirm if it is a vascular structure is to check and compare with the T1W sequence. The vascular structures are surrounded by interstitial tissue and fat, through the T1W sequences we will see the vascular structure together with a white line, in relation to fat.
Recommendations for assessing muscle MRI
Our recommendation is to start with a sensitive liquid sequence in a coronal or sagittal plane. In these sequences, the acute muscular pathology is hyperintense (shines) due to the presence of free fluid, they are “snitch” sequences that immediately allow us to detect where the problem is. Starting with the coronal or sagittal plane, is simply because they are planes that cover a greater assessed region (greater field of view) and help us to get an overview of the injury and its impact on the tension of the connective tissue and the pennation angle of the muscle fibres.
If the DICOM viewer that we use to visualize the images allows us to work with a display of several views, it is advisable to assess the images in different projections at the same time together with a reference line, to better locate the injury topographically and to confirm in different planes fibrillar tears of connective and muscular tissue.
Radiologists are known for assessing the explorations following a constant method. In the case of muscle MRI, we start with the tendon, we continue through the MTJ (tendon-aponeurosis, muscle) and myofascial junction (muscle and extra muscular space). Once we have assessed the injured myoconnective junction, we must assess secondary findings such as:
- Scars close to the injury (distortion of the histoarchitecture characterized by a markedly hypointense area in all sequences, with adjacent fatty component and retraction).
- Surgical history (also characterized by an architectural distortion together with images of ferromagnetic artifacts, images of a very hypointense signal that do not present a normal anatomical morphology).
- Vascular bundles included in the lesion.
- Nerve structures (i.e. sciatic nerve) that may suffer a retraction due to adhesions secondary to the healing of muscle injury.
- Possible anatomical abnormalities, accessory muscles, abnormal divisions or abnormal distribution of the connective tissue.
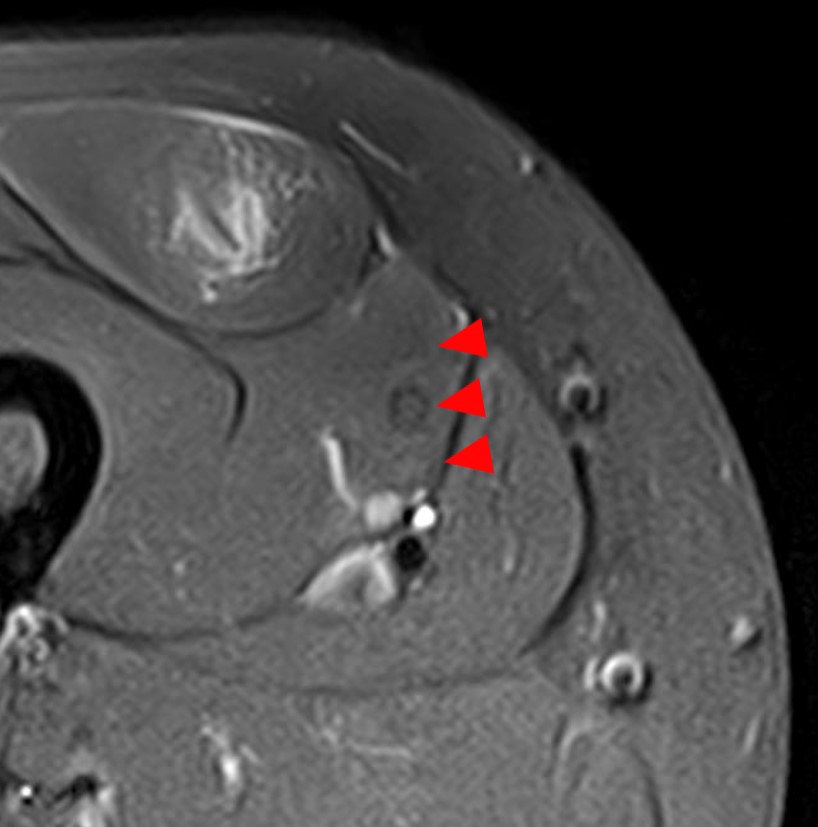
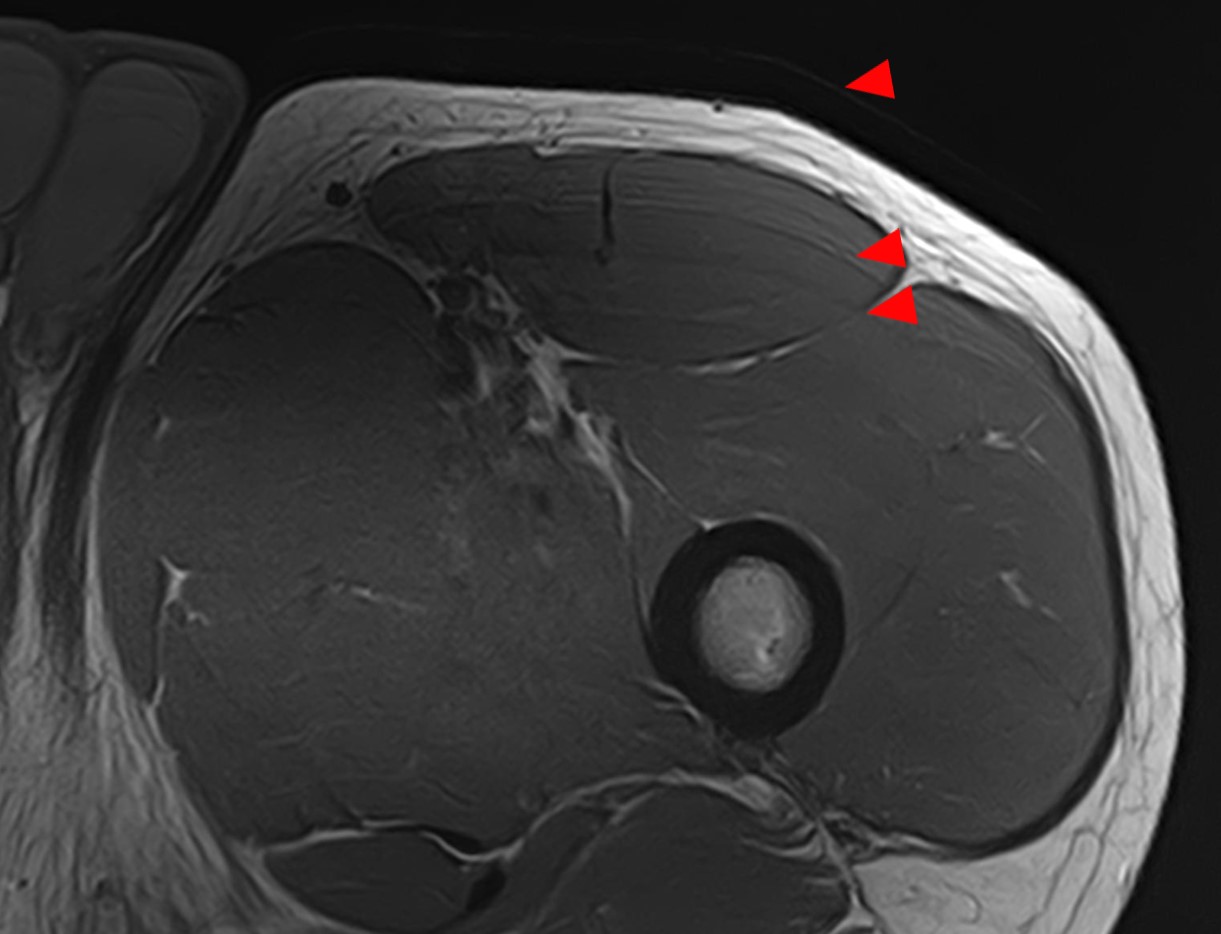
We should pay attention to the pulsatile flow artifacts, round heterogeneous images consecutively repeated in one direction and they are in close relation to vessels. We can consider them as signal muscle fibres anomalies when they are not real images (Fig. 3). Another typical artifact that we can find in the muscle MRI is the motion artifacts. Parallel lines localized outside the body that are associated with a diffuse blurring of the image and this leads to difficulties in the analysis of the image (Fig. 4). When we see these images, we have to analyse the whole section just to detect the outside extension of these artifacts.
Muscle MRI is also useful in the follow-up.
If the reason for the examination is not an initial diagnosis but an assessment of the evolution of the scar healing tissue, the MRI can tell us if the scar maturation is adequate and if the injured MTJ is adapting correctly to the scar. At the same time, we can assess complications such as large haematomas or gross scars that can suppose a difficulty in the correct adaptation of the muscle to the new healed myoconnective junction.
Muscle MRI is part of the diagnostic algorithm for most muscle injuries, as well as their follow-up. On many occasions, images are considered radiological signs of pathology when they are just normal anatomical structures with whose behaviour in MRI is not sufficiently known. With this article we intend to help reduce these misinterpretations. But it should never be doubted that to provide an optimal care it is necessary that the interpretation of the findings be made by a multidisciplinary team made up of radiologists, sports doctors, orthopaedic surgeons and physiotherapists.
Authors:
Sandra Mechó – Musculoskeletal Radiologist. FCBarcelona and Hospital de Barcelona.
Carles Pedret – Sports Medicine and Sports Orthopedics MD, PhD. Musculoskeletal Sonographer
BIBLIOGRAPHY:
Ekstrand J, Hägglund M, Waldén M. Epidemiology of Muscle Injuries in Professional Football (Soccer) Am J Sports Med 2011; 39: 1226-1232
Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional fooball players: A 10-year review. Am J Sports Med 2011; 39: 843– 850
Balius R, Blasi M, Pedret C et al. A Histoarchitectural Approach to Skeletal Muscle Injury. The Orthopaedic Journal of Sports Medicine 2020; 8(3)
Peña-Amaro J. The musculotendinous transition of the extracellular matrix. Apunts Sports Medicine 2021; 56.
Isern-Kebschull J, Mechó S, Pruna R et al. Sports-related lower limb muscle injuries: pattern recognition approach and MRI review. Insights into Imaging 2020;11:108
Flores DV, Mejía Gómez C, Estrada-Castrillón, Smitaman S, Pathria MN. MR Imaging of Muscle Trauma: Anatomy, Biomechanics, Pathophysiology, and Imaging Appearance. Radiographics 2018; 38: 124-148.
Guermazi A, Roemer FW, Robinson P, Tol JL, Regatte RR, Crema MD. Imaging of Muscle Injuries in Sports Medicine: Sports Imaging Series. Radiology 2017; 282(3): 646-663
Lee JC, Mitchell AWM, Healy JC. Imaging of muscle injury in the elite athlete. The British Journal of Radiology. 2012; 85: 1173-1185
Chen Y, Haacke EM and Li J. Peripheral nerve magnetic resonance imaging [version 1]. F1000Research 2019, 8(F1000 Faculty Rev):1803