Name of the mobile application: PowerFrail.
Category of the mobile application: Health.
Platform: Android (4.3 or later), iOS (8.2 or later, in process),
Cost: Free.
About the app
PowerFrail is an evidence-based application designed to assess relative muscle power (i.e. muscle power normalized to body mass) and frailty in older people, and to provide individualized goals of exercise training and physical activity based on the data recorded.
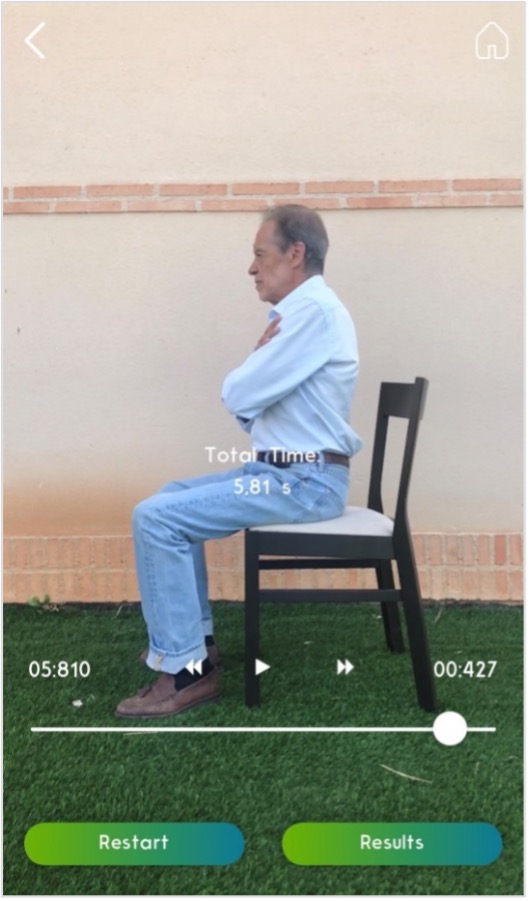
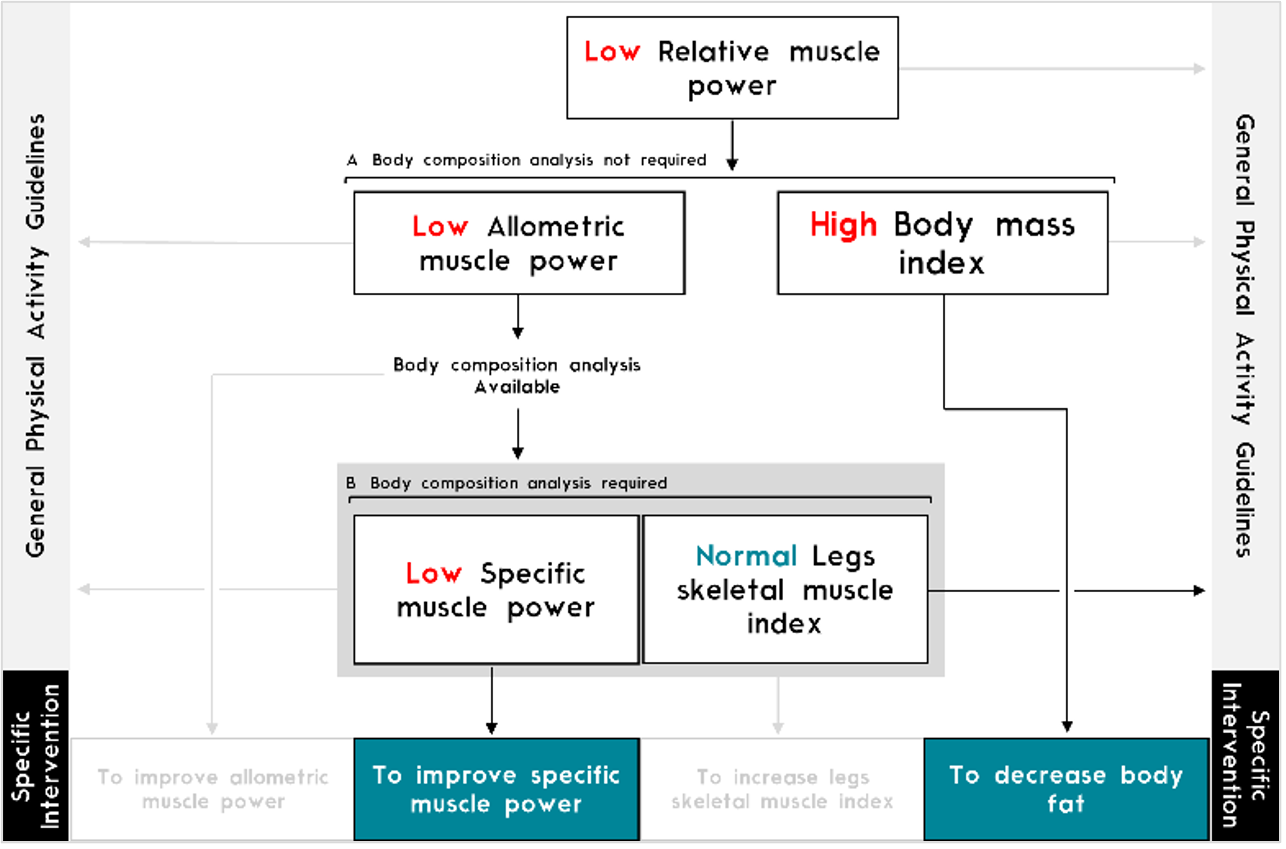
PowerFrail assesses relative muscle power by means of the validated sit-to-stand (STS) muscle power test (1, 2). Briefly, PowerFrail registers individuals’ anthropometric information and STS performance, which can be either video recorded (Figure 1) or entered directly by the user. Then, PowerFrail uses a validated equation that transforms STS performance into relative muscle power. Finally, based on normative data and cut-off points obtained from four European cohorts of older people, PowerFrail determines whether relative muscle power is low, and which individual features should be improved in that case (e.g. allometric power, body mass index, specific power or leg muscle mass) as PowerFrail incorporates an operational definition and algorithm of low relative muscle power (3). Of note, PowerFrail can be used with any version of the STS test (e.g. 5-rep STS test or 30-s STS test).
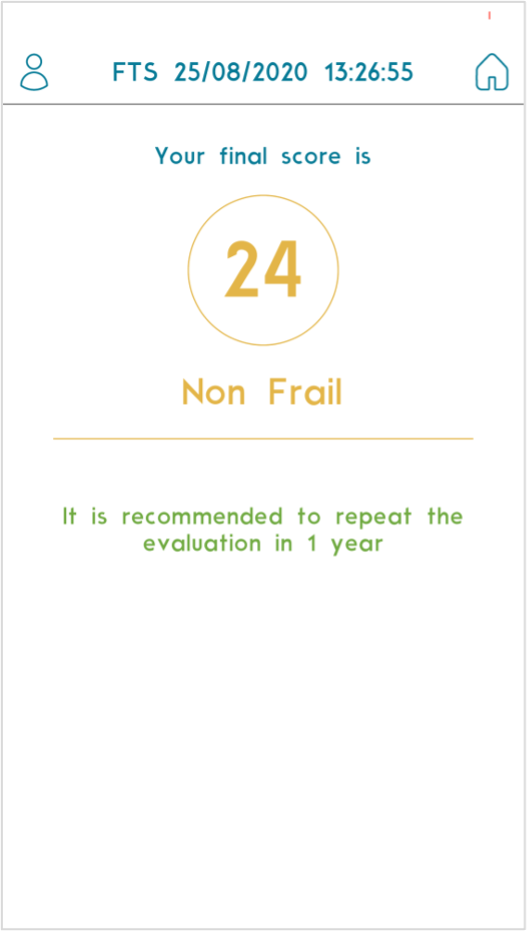
Furthermore, PowerFrail evaluates frailty using the validated Frailty Trait Scale-Short Form (FTS-5) (4). This frailty instrument recently created for clinical practice assesses the degree of frailty (from 0 [no frailty] to 50 [maximum frailty]) through five items: body mass index, balance, handgrip strength, gait speed and physical activity. PowerFrail integrates a step-by-step process by which each of these domains is recorded. Finally, PowerFrail provides an FTS-5 score, and physical activity recommendations based on the degree of frailty.
Importantly, the entered and recorded information is saved by PowerFrail, and the final report obtained from each test can be consulted when required. The feasibility and usefulness of PowerFrail make this mobile application a potentially adequate choice in multiple health-related settings (e.g. clinical, research and public health).
Use in clinical practice
The World Health Organization has encouraged health systems to prioritize the healthy aging goals of maintaining and improving functional ability. Low relative muscle power has been associated with mobility limitations, frailty, disability, poor quality of life and all-cause mortality among older adults. However, the assessment of muscle power is currently underused in the clinical setting. PowerFrail incorporates an operational definition and algorithm of low relative muscle power (Figure 2) and provides a feasible and validated tool for its assessment in the clinical setting.
In addition, frailty has been declared an emerging public health priority. PowerFrail facilitates the assessment of frailty by a five-step procedure, which yields a punctuation instead of classifying the patients into categories (Figure 3). The latter allows the monitoring of frailty trajectories among older adults with higher sensitivity. Finally, the recommendations provided by PowerFrail can help practitioners make better decisions with their patients.
- Free, portable, easy, and fast procedure to assess muscle power and frailty in older adults.
- All required calculations for obtaining relative muscle power (and its derivatives) and frailty are carried out by PowerFrail.
- Feedback provided by PowerFrail is based on normative data and cut-off points obtained from data from >10000 older people.
- Multiple language support (English and Spanish).
- Can be used in telemedicine.
Cons
- The determination of specific power and leg skeletal muscle index requires the external assessment of leg muscle mass, which can be entered in PowerFrail.
- The assessment of handgrip strength requires specialized equipment (a handheld dynamometer).
- The parameters of the exercise programs must be prescribed by an exercise specialist.
Authors and Affiliations:
Julian Alcazar1,2, Ignacio Lopez-Moranchel1,2, Jose Losa-Reyna1,2,3, Ivan Baltasar-Fernandez1,2, Francisco J. Garcia-Garcia2,3, Luis M. Alegre1,2, Ignacio Ara1,2
- GENUD Toledo Research Group, Universidad de Castilla-La Mancha. Toledo, Spain.
- CIBER of Frailty and Healthy Aging (CIBERFES), Instituto de Salud Carlos III. Madrid, Spain.
- Department of Geriatrics, Hospital Virgen del Valle, Complejo Hospitalario de Toledo. Toledo, Spain.
Twitter: @JulianAlcazar_ ; @LopezMoranchel ; @JoseLosaReyna ; @IvanBaltasar ; @Luismalegre ; @iara_royo
Conflicts of interest
The authors declare no conflicts of interest.
References
- Alcazar J, Kamper RS, Aagaard P, Haddock B, Prescott E, Ara I, et al. Relation between leg extension power and 30-s sit-to-stand muscle power in older adults: validation and translation to functional performance. Sci Rep. 2020;10(1):16337.
- Alcazar J, Losa-Reyna J, Rodriguez-Lopez C, Alfaro-Acha A, Rodriguez-Manas L, Ara I, et al. The sit-to-stand muscle power test: An easy, inexpensive and portable procedure to assess muscle power in older people. Experimental gerontology. 2018;112:38-43.
- Losa-Reyna J, Alcazar J, Rodríguez-Gómez I, Alfaro-Acha A, Alegre LM, Rodriguez Manas L, et al. Low relative mechanical power in older adults: an operational definition and algorithm for its application in the clinical setting. Experimental gerontology. 2020;141:111141.
- García-García FJ, Carnicero JA, Losa-Reyna J, Alfaro-Acha A, Castillo-Gallego C, Rosado-Artalejo C, et al. Frailty Trait Scale-Short Form: A Frailty Instrument for Clinical Practice. Journal of the American Medical Directors Association. 2020;21(9):1260-6.e2.