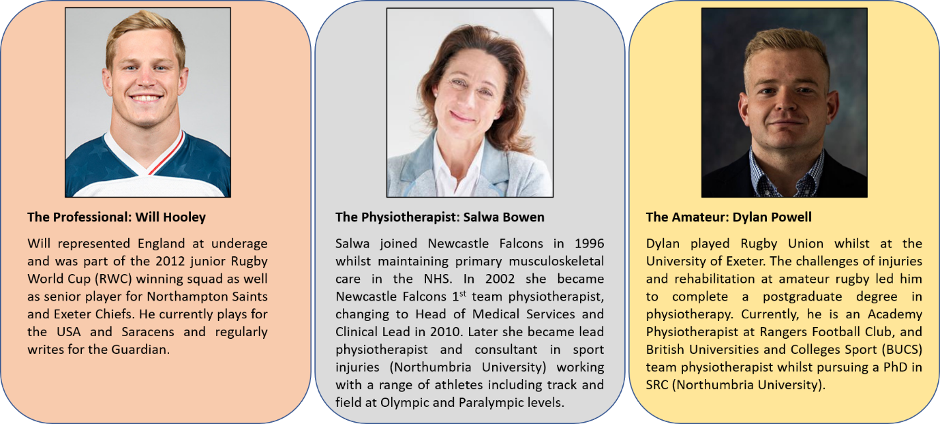
When it comes to concussion, return to play (RTP) before full recovery increases the risk of secondary injury. Heterogeneity in progression of symptoms and recovery times makes it difficult to determine when it is safe to RTP1,2. Considerable focus is given to the professional game but there remain inadequate considerations at amateur level. We present the perspectives of three different stakeholders on concussion in men’s rugby union in this blog.
PERSPECTIVES
The Professional Rugby Player’s Perspective
All players in the top two leagues are required to study and complete an RFU concussion tutorial which educates players around diagnosis, rehabilitation pathway and RTP. This includes understanding the Head Injury Assessment protocol and tests such as Sport Concussion Assessment Tool (SCAT)3 to better appreciate diagnosis and the rehabilitation pathway.
Outline the management you received after a concussion?
I sustained a concussion while representing USA against England at the 2019 senior rugby world cup. I was knocked unconscious and have no recollection of the incident. I do recall that I received a CT scan to rule out other injuries. The medic in charge (neutral match day doctor) assessed me and was there throughout my hospital assessment. After concussion symptoms were resolved (3-days), I was able to complete a 20-minute low intensity cycle. After completing further SCAT3 tests, I returned to training with controlled contact. I missed the French game but within 13 days I was playing against Argentina. I saw the medical team at least once/day right up until playing.
What can be transferred into the amateur game?
The problem with the amateur game is lack of finance. What I described previously relies on money being spent to source needs. I believe that all clubs should get registered players to complete a baseline concussion assessment and there should be a medical professional at all levels of rugby matches. As a result of players investing time to complete a concussion assessment, and having a medical professional present, amateurs may take concussion more seriously. They will understand what they are dealing with and help their teammates to understand. They may then be more rigorous in their recovery and will recognise the importance of dealing with concussion.
What would you want all medics to know/appreciate for RTP post-concussion?
Due to a player being in the heat of the moment, it is important for medics to have the ability to override the player’s emotion/willingness to stay on the pitch or RTP post-concussion. Due to the competitive nature of the player s/he will try and hide symptoms, feelings and even altering body language as processes very much rely on ‘how the player feels’. Sometimes players push themselves too hard and lie about their symptoms to enable them to RTP. Alternatively, players can also overthink how they are feeling, making them feel worse than they are. Naturally, players want to continue playing/training and so medics must see through these.
The Physiotherapist’s Perspective
Professional rugby union
Regular daily contact with the doctor or physiotherapist at this level, identifies and monitors ongoing (or delayed) symptoms of concussion. Early action is taken to manage the player. Referrals are made to a neuroscience department with a consultant when appropriate. This helps minimise stress/anxiety and the potential psychological implications of the inability to compete without a time frame. Dealing with low mood and depression associated with being removed from play, becomes part of the management plan with positive coping strategies being introduced early in the management process.
Amateur rugby union
‘Recognise and remove’ is the protocol for management and identification of a potential concussion, based on a cautious approach. The landscape in amateur/university sport is very different in concussion management from one club/university to another. Daily contact with a physio is not always possible with a player due to their other commitments. S/he may be managed by different practitioners through the graduated RTP process and so there is no consistency within the clinical judgement. Lack of consistency can make management of more complex cases very difficult.
The Amateur Rugby Perspective
My team experienced a few concussions during 2019-20, one was in Wales and required hospital assessment. The coach and player were in A&E for 12-hours before treatment. The alternative was to return to the north east (7-hr), making it challenging to monitor the athlete and note any deterioration. This is common within BUCS (top level UK university competition) rugby and players often feel that they are given non-specific concussion advice and discharged home. Some players recognise concussion is a serious injury but most do not want to be removed from play/training, remaining unaware of the damage they may be doing by playing on. BUCS Super Rugby is an amateur league, which is arguably operating at a semi-professional level as it aims to provide a pathway for aspiring professionals. Managing concussion in this competition raises many challenges but may provide opportunities to better facilitate our future understanding, diagnosis and treatment of concussion.
What is there to learn?
Education and communication on the significance of concussion management is key. Elite level players are required to undertake formal concussion learning, appearing to be well received and respected at professional levels. There might be demand for this within the amateur/university game and it should be more robustly conveyed to younger athletes.
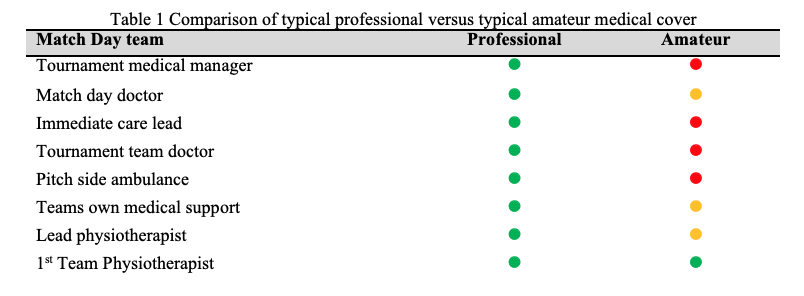
There are differences in the availability of resources for professionals and amateurs, as seen in Table 1. In terms of participation, professional and registered club players only represent a minority of players (6.5%) compared to the 1.9 million amateurs4. A rebalancing of resources is key to increase medical provision for amateurs, e.g. mandatory PHICIS level 2 course for all physios. There is a need to better understand the occurrence and dynamics of concussion in amateur rugby because of the lower availability of medical professionals.
Authors and Affiliations:
Dylan Powell, Department of Computer & Information Science, Northumbria University, Newcastle Upon-Tyne
Salwa Bowen, Northumbria Sport, Northumbria University, Newcastle Upon-Tyne
Will Hooley, Saracens Rugby Club, England
Sam Stuart, Department of Health and Life Sciences, Northumbria University, Newcastle Upon-Tyne
Alan Godfrey, Department of Computer & Information Science, Northumbria University, Newcastle Upon-Tyne
Competing interests None Declared
References:
- McCrory et al. 2016. Br J Sport Med. 12(1):6–11.
- World Rugby. 2018. http://playerwelfare.worldrugby.org/concussion
- Sports Concussion Assessment Tool 2017 https://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097506SCAT5.full.pdf
- World Rugby 2017, https://www.world.rugby/development/player-numbers?lang=en Accessed February 2020
- World Rugby Tournament Minimum Medical Standards 2019 https://www.world.rugby/news/407666?lang=en Accessed February 2020
Funding info This work was funded by Northumbria University as part of doctoral research programme (D Powell). The work was also supported by the Private Physiotherapy Education Fund (PPEF, RPJ03732)