Current physical activity guidelines for adults aged 18 to 65 years suggest at least 150 minutes per week of moderate intensity aerobic activity (e.g. a brisk walk for 30 minutes 5 times per week). Walking is a popular form of active transportation and it’s also a great workout! Many of us walk as a form of physical activity because it is an aerobic exercise that does not require special equipment and offers numerous health benefits. Unfortunately, knee osteoarthritis is a major contributor to walking difficulty1. Only a small proportion of people with knee osteoarthritis achieve the recommended amount of physical activity2—perhaps because of pain or fear that too much activity is harmful for their already painful knees. The facts are, however, physical activity is good for our joints, exercise can actually decrease pain if you stick with it3, and it has other important positive effects on health and wellbeing.
A role for measuring cadence?
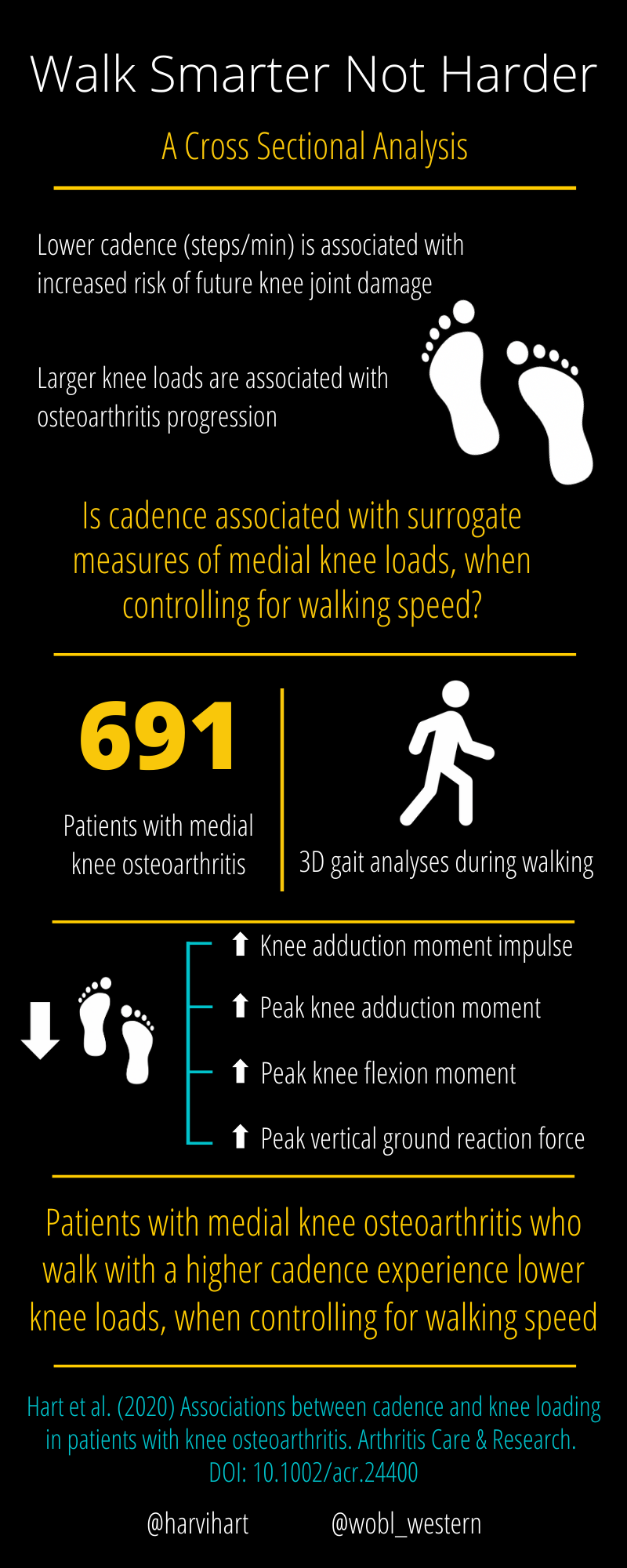
Walking cadence, aka step rate, is defined as the total number of steps one takes in a minute. Cadence is a practical way of monitoring the intensity of walking. In general, walking at approximately 100 steps per minute is suggested for adults to achieve moderate intensity physical activity4. People with knee osteoarthritis often walk with a lower cadence (i.e., fewer, longer steps). My previous research suggests there is an association between walking cadence and future joint damage measured on MRI5. Using data from a large longitudinal cohort study, our study showed that people with or at risk of knee osteoarthritis who walked with a lower cadence experienced more joint damage over time. The proposed mechanism was that lower cadence resulted in prolonged knee loading, which increased knee articular cartilage degeneration. The concept is similar to that proposed for runners, where running with a higher cadence is associated with lower measures of knee loading6.
In my most recent study, we set to test this hypothesis. We hypothesized that higher walking cadence would be associated with lower knee loads in people with knee osteoarthritis7. We used three-dimensional gait analysis to measure knee moments (i.e. angular forces) in the frontal plane during walking to provide indirect, surrogate measures of knee cartilage load. As knee adduction moment angular impulse—a proxy measure of medial knee load that takes into account both the magnitude and the duration of stance—has been associated with progression of joint damage8 and with knee pain, we focused on knee adduction moment angular impulse (from here on I refer to it as medial knee loading). Our results suggested that higher cadence (i.e., more, shorter steps), when controlling for walking speed, is associated with lower medial knee loading. Every extra step per minute was associated with 0.02%BW.Ht.s (normalized to percent bodyweight times height times seconds) decrease in knee medial knee loading. A typical patient in our study would take on average 100 steps per minute and experience 1.6 %BW.Ht.s of medial knee loading. Let’s say we ask them to increase their cadence by 20 steps per minute, so instead of taking 100 steps per min they now take 120 steps per minute. Based on our findings, 1 step/minute increase in cadence was associated with 0.02 %BW.Ht.s decrease in medial knee loading—so the extra 20 steps/min would equate to 0.4%BW.Ht.s decrease in medial knee loading, from 1.6 to 1.2%BW.Ht.s. In other words, if the patient walked at the same walking speed, but increased their cadence by 20%, our results suggest that medial knee loading would decrease by approximately 25%, per step.
Given the positive effects of physical activity and the negative effects of excessive medial knee loading, this work supports the need for future research. Studies testing gait adaptations using metronomes, verbal cues, smartphones/smart watches, etc. to increase cadence may show they help manage knee loading in people with knee osteoarthritis and enable them to walk more and meet their walking targets.
For a podcast on the topic with Dr Hart – see the link below
Author:
Harvi Hart, Ph.D.
@harvihart
References
- King, L.K., et al., Impact of Osteoarthritis on Difficulty Walking: A Population-Based Study. Arthritis Care & Research, 2018. 70(1): p. 71-79.
- Wallis, J.A., et al., What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthritis Cartilage, 2013. 21(11): p. 1648-59.
- Fransen, M., et al., Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev, 2015. 1: p. Cd004376.
- Tudor-Locke, C., et al., How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. British Journal of Sports Medicine, 2018. 52(12): p. 776-788.
- Hart, H.F., et al., Step Rate and Worsening of Patellofemoral and Tibiofemoral Joint Osteoarthritis in Women and Men: The Multicenter Osteoarthritis Study. Arthritis Care Res (Hoboken), 2020. 72(1): p. 107-113.
- Lenhart, R.L., et al., Increasing running step rate reduces patellofemoral joint forces. Med Sci Sports Exerc, 2014. 46(3): p. 557-64.
- Hart, H.F., et al., Associations between cadence and knee loading in patients with knee osteoarthritis. Arthritis Care Res (Hoboken), 2020. https://doi.org/10.1002/acr.24400
- Bennell, K.L., et al., Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis, 2011. 70(10): p. 1770-4.