Part 2 of a 4 part blog series by Dr John Orchard
The example of corticosteroids for knee OA
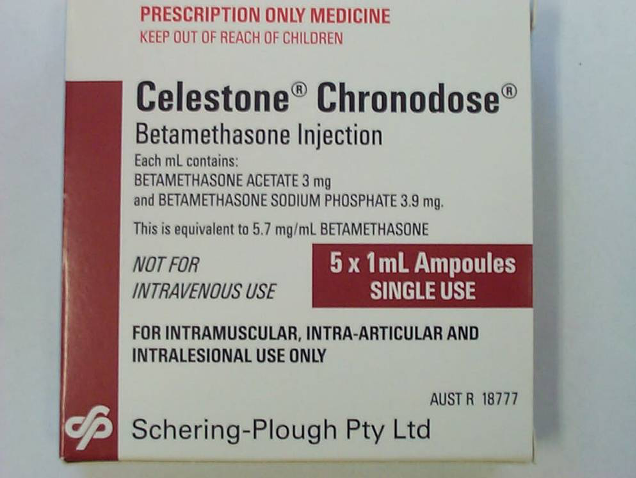
The focus of this episode on the use of cortisone injections (IAC = intra-articular cortisone) for knee osteoarthritis (OA), which I wrote about in an Education review in BMJ earlier this year1. Cortisone injections are commonly used for knee OA on the back of mild transient improvements2. This Cochrane review 2 reported likely mild benefit of very short duration based on generally low-quality (high risk of bias studies). It made it clear there was very little long-term data – as of 2015 – and no evidence for any benefit other than in the very short-term. So important to state there are no studies showing any medium to long term benefit of IAC for knee OA.
Recent studies show consistent and conclusive results
Between 2017-2020 there have been at least ten original, independent studies (Table 1 below, updated from the Table in the BMJ review1), fully peer-reviewed and published in high ranking journals investigating the long-term effects of IAC. All studies show an association of IAC use and either worse outcome than comparator or harm in the long-term for knee OA. I appreciate that all ten of these studies have limitations, detailed in the Table. But I repeat neither any of the ten nor any other studies have shown any benefit of IAC in the long-term for knee OA. There is one placebo-controlled RCT, one physio-controlled RCT, one PRP-controlled RCT, 5 cohort studies with varied attempts to control for confounding, one case control and one large uncontrolled case series assessing harms. Generally, the author groups are distinct. In addition a systematic review3 is published with a focus on long-term benefits of knee OA treatments and states unequivocally that IAC has no long-term benefit in knee OA.
Table 1 shows the tsunami of negative evidence for long-term outcomes of IAC for knee OA from 2017-2020, which I consider totally decisive coming on top of the background that there has never been any evidence of long-term benefit.
Cortisone for knee arthritis is a medical reversal that needs to happen, and we really need to critically assess not only medical education but also the process for expert consensus statements as to why there is so much resistance to admitting when we’ve got it wrong. I will expand on this in two further blogs over the coming weeks…
| Study | Focus | Key Findings | Limitations (JO) | Conclusions trying to be balanced about both the findings and limitations of these articles. |
| Davis 2019 4 Nested cohort study of 1935 patients | Patients at risk of but without radiographic knee OA followed for 8 years to assess development of either knee OA or accelerated knee OA | Patients who underwent any procedure (injection or knee arthroscopy) or took pharmaceuticals were all more likely to develop accelerated knee OA. The relationship was particularly strong for knee arthroscopy and IAC (P<0.001) | Non-randomised study, and clearly confounding factors not accounted for may have increased risk of both knee OA and likelihood of undertaking treatment | Both IAC and knee arthroscopy are associated with (but did not necessarily cause) an increased risk of accelerated knee OA occurring in patients without radiographic OA |
| Deyle 2020 5 RCT in NEJM of 156 patients comparing physical therapy and IAC injections | Single-blinded RCT comparison between IAC and physical therapy for knee OA patients | Physical therapy patients had significantly greater improvement at 1 year follow-up than IAC patients | The physical therapy intervention was “mixed” (combination of hands-on treatment and exercise-based). There was no placebo control group. | This trial could be interpreted as being either supportive of combination physical therapy or, alternatively, a warning that IAC may not yield as good a result as a comparator treatment |
| Mackowiak 2020 6 Retrospective cohort study of 126,000 insurance claim patients | Comparison of ongoing costs between knee OA patients who were treated with (only) IAC or knee arthroplasty or hyaluronan injections | Hyaluronan injection patients had significantly fewer costs, requirements for ongoing painkillers or adverse events over 4 years than either IAC or knee arthroplasty patients. Compared to knee arthroplasty patients, IAC patients had fewer adverse events and medical costs in the first year of follow-up, but more adverse events and use of painkillers in years 2-4. | Non-randomised. Funded by a company which manufactures a hyaluronan injection, which may have biased the study | Although this was promoted by the authors as a cohort study supportive of hyaluronan injections, it equally could be read as a warning against the short-term harms of knee arthroplasty and the longer-term harms of IAC |
| Wijn 2020 7 Cohort study of 4796 patients | Patients with or at risk of knee OA followed for 9 years, comparing risk of requiring knee arthroplasty for those who used IAC to those who did not | Each IAC injection increased the absolute risk of arthroplasty by 9.4% at nine years’ follow-up compared with those who did not receive injections | Non-randomized study, with the possibility that those patients more willing to undertake injections were more willing to undertake arthroplasty | Possible that IAC leads to an increase in risk of long-term worsening of knee OA, resulting in higher rates of knee arthroplasty |
| McAlindon 20178
Randomized controlled trial |
Medium-term (3 months to 2 years) efficacy and safety
(140 patients) |
Intra-articular triamcinolone injection every 3 months resulted in greater cartilage volume loss detected on MRI at 2 years than did saline for a mean change in index compartment cartilage thickness of -0.21 mm vs -0.10 mm (between group difference -0.11mm, 95% CI -0.20 to -0.03mm). There was no clinically important difference in pain (-1.2 vs -1.9, between group difference 0.6, 95% CI -1.6 to 0.3). | Measurements were only made 3 months after each injection and could possibly have missed short-term improvements of IAC over placebo.
|
IAC provided no benefit over placebo in time frames from 3 months to 2 years, but was associated with progressive cartilage deterioration |
| Liu 2018 Cohort study9
(412 patients) |
Long-term effectiveness (2 years) as assessed by symptoms compared to controls | Compared to non-users participants initiating CSI experienced worsening of pain (yearly worsening: 1.24 points, 95% CI 0.82-1.66 on the WOMAC 20 point scale), along with worsening of stiffness and physical functioning after adjusting for potential confounders. | Cohort design rather than RCT is less powerful at eliminating confounders | IAC was associated with worsening symptoms over 2 years follow up |
| Zeng 201910 Cohort study
(148 IACs initiators, 536 comparators) |
Radiographic progression of knee osteoarthritis with IAC compared to controls (propensity-score matched) | Compared to non-users, hazard ratios (HRs) of joint structure worsening over 48 months from IAC initiation and continuous IACs were 3.02 (95% CI, 2.19-4.16) and 4.67 (95% CI, 2.92-7.47), respectively. | Cohort design rather than RCT is less powerful at eliminating confounders | CSI was associated with increased risk of structural deterioration and progression to knee replacement |
| Kompel 201911 Case series of 459 patients | Rate of rapid progression of hip and knee OA cases after guided IAC | 8% of knee OA cases exhibited rapid deterioration within 2 years of IAC | No control group | Study has several limitations but warrants further investigation |
| Pelletier 2020 12 Case-control study | Structural changes on MRI scan after IAC | No change in articular cartilage thickness but a change in meniscal thickness | Case-control methodology not ideal for assessing structural deterioration | Shows a single change (reduction in meniscal thickness) but which is in keeping with others that flag deterioration of joint integrity after IAC |
| Elksniņš-Finogejevs 2020 13 RCT between PRP and IAC | RCT comparing Platelet Rich Plasma (PRP) injection with cortisone injection >12 month follow up. | PRP had superior VAS, KSS and IKDC scores at 15, 30 and 58 weeks to cortisone. In addition 3/20 IAC patients elected to have knee replacement within the year (0/20 for PRP) | Non blinded study and no placebo group. Small sample size albeit statistical significance reached showing large difference between the groups | Doesn’t differentiate between possibility that PRP is placebo and IAC is harmful relative to placebo, or that both groups may be beneficial, with PRP being of greater benefit to IAC |
| Gregori 20183 Systematic review of all pharmacological interventions for knee OA
(33 interventions, 47 RCTs, 22037 patients) |
Long term pain control (>12 months) | Intermittent IAC injections were not associated with pain improvement in the long term. Combination with hyaluronic acid injection had moderately beneficial but variable effect on pain. | Very few studies examine medium to long-term effect of IACs alone | Based on limited evidence, IAC was not associated with pain improvement beyond 12 months |
| Conclusion | Multiple long-term studies assessing IAC for knee OA from 2017-2020, some RCT and many cohorts adjusted for confounding | There is no benefit for IAC for knee OA in the longer term, but it is associated with cartilage degeneration, worsening clinical outcomes and a higher risk of progressing to knee replacement | There is not (yet) a smoking gun 5-10 year follow-up RCT showing all of these negative associations in a single study | With no long-term benefit and now a large number of studies showing worse outcomes than placebo and other comparators, IAC cannot be recommended as a treatment for knee OA |
Join us next week for part 3 of 4!
Author and Affiliations:
John Orchard @DrJohnOrchard AM MD PhD FACSEP FFSEM (UK) FACSM
References:
- Orchard JW. Is there a place for intra-articular corticosteroid injections in the treatment of knee osteoarthritis? Bmj 2020;368:l6923.
- Jüni P, Hari R, Rutjes A, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015:Oct 22;(10):CD005328.
- Gregori D, Giacovelli G, Minto C, et al. Association of Pharmacological Treatments With Long-term Pain Control in Patients With Knee Osteoarthritis: A Systematic Review and Meta-analysis. Jama 2018;320(24):2564-79.
- Davis JE, Harkey MS, Liu SH, et al. Adults With Incident Accelerated Knee Osteoarthritis Are More Likely to Use Pharmacological Treatment Options and Receive Arthroscopic Knee Surgery: Data From the Osteoarthritis Initiative. ACR open rheumatology 2019;1(6):359-64.
- Deyle GD, Allen CS, Allison SC, et al. Physical Therapy versus Glucocorticoid Injection for Osteoarthritis of the Knee. N Engl J Med 2020;382(15):1420-29.
- Mackowiak J, Jones JT, Dasa V. A comparison of 4-year total medical care costs, adverse outcomes, and opioid/prescription analgesic use for 3 knee osteoarthritis pain treatments: Intra-articular hyaluronic acid, intra-articular corticosteroids, and knee arthroplasty. Semin Arthritis Rheum 2020.
- Wijn SRW, Rovers MM, van Tienen TG, et al. Intra-articular corticosteroid injections increase the risk of requiring knee arthroplasty. The bone & joint journal 2020;102-b(5):586-92.
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. Jama 2017;317(19):1967-75.
- Liu SH, Dubé CE, Eaton CB, et al. Longterm Effectiveness of Intraarticular Injections on Patient-reported Symptoms in Knee Osteoarthritis. J Rheumatol 2018;45(9):1316-24.
- Zeng C, Lane NE, Hunter DJ, et al. Intra-articular corticosteroids and the risk of knee osteoarthritis progression: results from the Osteoarthritis Initiative. Osteoarthritis Cartilage 2019.
- Kompel AJ, Roemer FW, Murakami AM, et al. Intra-articular Corticosteroid Injections in the Hip and Knee: Perhaps Not as Safe as We Thought? Radiology 2019:190341.
- Pelletier JP, Raynauld JP, Abram F, et al. Intra-articular corticosteroid knee injection induces a reduction in meniscal thickness with no treatment effect on cartilage volume: a case-control study. Sci Rep 2020;10(1):13789.
- Elksniņš-Finogejevs A, Vidal L, Peredistijs A. Intra-articular platelet-rich plasma vs corticosteroids in the treatment of moderate knee osteoarthritis: a single-center prospective randomized controlled study with a 1-year follow up. Journal of orthopaedic surgery and research 2020;15(1):257.