Medical Reversals and the “Slow” Brain
One of the best ‘medical’ books of recent years is Ending Medical Reversal by Prasad and Cifu1; it is close to essential reading for all doctors, medical students and even health professionals. It is referenced in an important editorial just published in the BJSM 2. In addition, Ending Medical Reversal could be read in conjunction with a series of other non-medical books that can give the context as to why expert beliefs in medicine can be so flawed. The most important book in the genre is Thinking, Fast and Slow 3 but perhaps a more enjoyable read to illustrate the concept and the story of the geniuses behind it is The Undoing Project 4, by the author of Moneyball 5 and The Blind Side 6. Finally on this topic, Blink 7 should rate a brief mention – if only to illustrate that experts make most of their judgements within seconds, noting the important context as to how this sometimes leads to major flaws.
Medical Reversals and Musculoskeletal medicine
Prasad and Cifu 1 illustrate best when writing about Medical Reversals that have reached full conclusion – such as the removal from the market of Vioxx the dangerous anti-inflammatory [which was removed because it was the worst of a bad bunch, but which ignores the over-prescription and use of the multitude of other anti-inflammatories that increase cardiovascular mortality by an average of 30%8]. They also make some great suggestions about medical education and practice to reduce the likelihood of future medical reversals. In the musculoskeletal world (orthopaedics, rheumatology, sport & exercise medicine, physiotherapy etc) we are living in an enormous disconnect between evidence and practice for, sadly, the majority of musculoskeletal management. The knowledge of the disconnect has made very little difference to date to practice: musculoskeletal outcomes in most countries of the world are getting worse every year (think exponentially increasing knee replacements), because more medical management is actually harmful than helpful and health systems are not set up to stop harmful treatment from occurring. It would be nicer perhaps to work in a different medical field where there are more medical “wins” on the board. But even though Oncology, say, has many wins, Prasad (who is an Oncologist) is still very critical of his own specialty and much of the treatment within it.
Figure 1 – knee arthroscopy
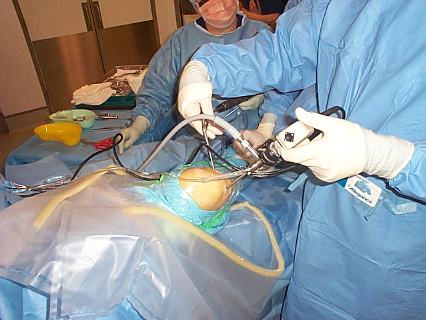
The example of knee arthroscopy
Prasad and Cifu – not being from musculoskeletal disciplines – wrote about knee arthroscopy in 2015 as a “reversal” without the full awareness that, yes, the evidence by 2015 had completely reversed9, but sadly the procedure is still in very common usage in most Western countries. The musculoskeletal specialists who aren’t orthopaedic surgeons now have a strong understanding of the evidence that knee arthroscopy does more harm than good2. But health systems still fund knee arthroscopy because they rely on the expert opinion of orthopaedic surgeons, many of whom are yet to accept this evidence. But at least the medical literature is full of expert calls to cease knee arthroscopy10 even if health funding systems primarily haven’t yet accepted the evidence. I can proudly claim to have perhaps been one of the first to question the funding of knee arthroscopy in the peer-reviewed literature in 200211, immediately after the initial RCT showing no benefit over placebo12. The recent editorial of Ardern et al.2 perfectly illustrates the mechanisms that have led to a reduction in knee arthroscopy in countries with primarily socialised medicine. In a “fee-for-service” market like my own medical system in Australia, ongoing funding of knee arthroscopy means that surgeons who continue to practice in a “non-evidence-based” fashion earn higher salaries than those who follow evidence-based practice. In health systems like Australia and the USA, if funding of ineffective procedures is not addressed, it eventually may be another mechanism of capitalist systems, namely class-action lawsuits, that could finally put an end to harmful knee arthroscopies. It is not simply knee arthroscopy though; for knee osteoarthritis in general health systems fund too much of what it harmful and not enough of what helps 13. A follow-up Blog will examine cortisone injections for knee osteoarthritis as an equal part of the problem.
Join us next week for part 2 of 4!
Author and Affiliations:
John Orchard @DrJohnOrchard AM MD PhD FACSEP FFSEM (UK) FACSM
References
- Prasad V, Cifu A. Ending Medical Reversal: Improving Outcomes, Saving Lives. Baltimore: John Hopkins University Press, 2015.
- Ardern C, Paatela T, Mattila V, et al. When taking a step back is a veritable leap forward. Reversing decades of arthroscopy for managing joint pain: five reasons that could explain declining rates of common arthroscopic surgeries. Br J Sports Med 2020;54:1312-13.
- Kahneman D. Thinking, Fast and Slow: Farrar, Straus and Giroux, 2011.
- Lewis M. The Undoing Project: A friendship that changed our minds: W. W. Norton Company, 2016.
- Lewis M. Moneyball: The Art of Winning an Unfair Game. ISBN 0-393-05765-8: W.W. Norton & Company, 2003.
- Lewis M. The Blind Side. Evolution of a game. ISBN 978-0393330472: W.W. Norton & Company, 2007.
- Gladwell M. Blink: the power of thinking without thinking: Back Bay Books, 2005.
- Bally M, Dendukuri N, Rich B, et al. Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. Bmj 2017;357:j1909.
- Thorlund JB, Juhl CB, Roos EM, et al. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. Bmj 2015;350:h2747.
- Mounsey A, Ewigman B, Hickner J. Arthroscopic surgery for knee osteoarthritis? Just say no. Journal of Family Practice 2009;58(3):http://www.jfponline.com/pdf%2F5803%2F03JFP_PURL.pdf.
- Orchard J. Health insurance rebates in sports medicine should consider scientific evidence [editorial]. J Sci Med Sport 2002;5(4):v-viii.
- Moseley J, O’Malley K, Petersen N, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 2002;347(2):81-8.
- Orchard J, Moen MH. Has reimbursement for knee osteoarthritis treatments now reached ‘postfact’ status? Br J Sports Med 2017;51(21):1510-11.