The health benefits of physical activity (PA) are well-established.1 One in four adults achieves less than 150 minutes of moderate-intensity PA per week2 at an estimated global healthcare cost of INT$54 billion.1 World Health Organization (WHO) member states agreed to reduce inactivity by 15% by 2030.1
WHO’s Global Strategy on Ageing and Health establishes lifelong PA as critical to prevent chronic disease, reduce healthcare burden and maintain functional capacity. 3 PA slows the physiological changes of ageing and improves health-related quality of life.3 Any increase in PA is worthwhile:1 muscle-strengthening and aerobic activity reduce mortality4, and exercise that targets balance and function prevents falls.5
Physical activity in middle-age
Middle-age (45-64 years) is an ideal time to be active. Large longitudinal studies have found that increased PA in middle-age delays disability by up to 15 years6 and that those with higher leisure-time PA at age 46 were 1.5 times more likely to have good perceived-health in older age.7 PA often decreases during middle-age, most likely due to employment, health and household/caregiving responsibilities.
Practical strategies to support middle-aged people becoming more active are urgently needed. The WHO Global Action Plan on Physical Activity strives to create active societies, environments, people, and systems that are safe and diverse.1 The ‘active people’ objective calls for “…opportunities and programmes, across multiple settings, to help people of all ages and abilities to engage in regular physical activity as individuals, families and communities.”1
Deliberations of an expert group
Our multidisciplinary panel determined priorities for PA promotion in middle-age at an in-person meeting (August 2018) and follow-up interviews. The panel consisted of senior clinicians and academics in public health, physiotherapy, musculoskeletal epidemiology, occupational therapy, rehabilitation medicine, neurology, geriatric medicine, rheumatology, health economics, and psychiatry. Our six priorities for PA promotion in middle-age are described in Figure 1. Key recommendations were then developed after discussion of the feasibility, acceptability and potential impact of each option.
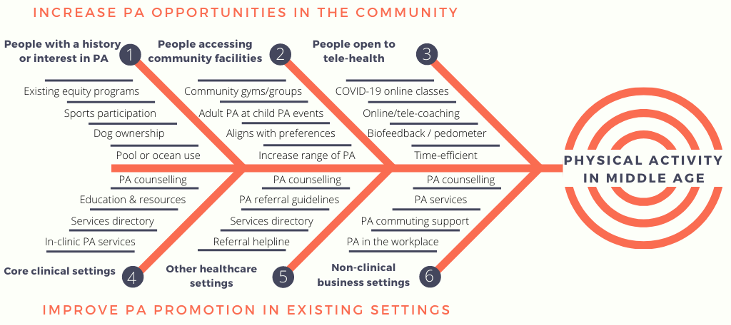
Three of our priorities target behavioural characteristics:
1. People with a history or interest in being active (e.g. previous sports engagement or dog ownership)
2. People accessing existing local community activities (e.g. sports clubs or community gyms)
3. People open to tele-health modalities (e.g. COVID-19 online classes).
In priority (1) we suggest that middle-aged people with a history or interest in being active have higher propensity for engagement with PA interventions that are time-efficient, close to existing work-, family-, or community activities. In priority (2), we determined that local community activities improved accessibility and time-efficiency for middle-aged people with limited healthcare contact. Leveraging such activities may also align with individual preferences, family activities and address perceptions of being ‘too busy to exercise’, as well as support disadvantaged groups and communities. In priority (3), we note evidence of the acceptability of tele-health and coaching in middle-age as a principle for intervention design and setting.
Three further priorities relate to settings:
4. Core clinical healthcare settings where PA counselling and referral could be central to the clinical interaction (e.g. hospital inpatient/outpatient)
5. Other clinical healthcare settings where PA counselling and referral could be adjunctive to the clinical interaction (e.g. primary care)
6. Non-clinical business settings (e.g. workplace or community PA providers).
In priority (4), we acknowledge the effectiveness of referral schemes for supporting core clinical services with education and resources, such as guidelines and service directories. In priority (5), we recommend development/adaptation of education and resources to support other clinical healthcare settings. In priority (6), we propose opportunities for PA promotion in non-clinical business settings, such as workplaces or through community providers.
We suggest the prioritisation of PA promotion as well as PA counselling and referral in healthcare settings because many middle-aged adults spend less time in clinical or educational settings, and are often working and tech-savvy, but time-poor with carer responsibilities. Therefore, program delivery in settings middle-aged people already access seems a sensible solution. We suggest targeting such people through: concurrent adult PA at children’s sport or schools; interests such as sporting or social clubs and workplaces; and telehealth at home. We consider it essential to implement the WHO’s Strategy on Ageing and Health and the Global Action Plan on Physical Activity and to call for investment in such initiatives.
Physical activity requires individual behaviour within a complex system.1 Capability, opportunity and motivation influence behaviour.8 PA promotion strategies that build on existing behaviours and settings could develop capability and provide opportunity. Motivation could be enhanced by better awareness of the PA benefits in terms of quality of life, physical function and independence in older age, as well as creating social norms and leverage community leaders and role models. Development and evaluation of such approaches is particularly needed if we are to achieve the global goals of healthy ageing and inactivity reduction – even more important now given the strain on health systems from COVID-19.
Authors and Affiliations:
| Dr Jennifer Taylor1,2
Kate Purcell1,2 Associate Professor Anne Tiedemann1,2 Professor Lisa Harvey3,7 Professor Adrian Bauman4 Professor Fiona Blyth4,11 Professor Roberta Shepherd6 Dr Leanne Hassett1,2,6 Professor Lindy Clemson9,10 |
Professor Ian D Cameron3, 8
Professor Colleen Canning6 Professor Susan Kurrle7 Professor Lyn March7,8,12 Professor Kirsten Howard2 Professor Allison Tong2 Professor Vasi Naganathan5,11 Professor Cathie Sherrington1,2
|
1Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia
2School of Public Health, Faculty of Medicine and Health, The University of Sydney, Australia.
3John Walsh Centre for Rehabilitation Research, Faculty of Medicine and Health, The University of Sydney, Australia
4Charles Perkins Centre, School of Public Health, Faculty of Medicine and Health, The University of Sydney, Australia
5Concord Clinical School, Faculty of Medicine and Health, The University of Sydney, Australia
6Discipline of Physiotherapy, School of Health Sciences, Faculty of Medicine and Health, The University of Sydney, Australia
7Northern Clinical School, Faculty of Medicine and Health, The University of Sydney, Australia
8The Royal North Shore Hospital, Northern Sydney Local Health District, St Leonards, Sydney, Australia
9ARC Centre for Excellence in Population Ageing Research, The University of Sydney, Australia
10Discipline of Occupational Therapy, School of Health Sciences, Faculty of Medicine and Health, The University of Sydney, Australia
11Centre for Education and Research on Ageing (CERA), Faculty of Medicine and Health, The University of Sydney, Australia
12Institute of Bone and Joint Research and Kolling Institute, Northern Sydney Local Health District and Faculty of Medicine and Health The University of Sydney, Australia
Corresponding author:
Jennifer Taylor: jfis8639@uni.sydney.edu.au ORCID: https://orcid.org/0000-0003-2152-4287
There are no competing interests.
References:
- WHO. More active people for a healthier world. 2018. World Health Organisation (WHO).
- Guthold R, Stevens GA, Riley LM, et al. Worldwide trends in insufficient physical activity from 2001
to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. The Lancet
Global Health 2018; 6: e1077-e1086. DOI: 10.1016/s2214-109x(18)30357-7. - WHO. Global strategy and action plan on ageing and health. 2017. World Health Organisation
(WHO). - Zhao M, Veeranki SP, Magnussen CG, et al. Recommended physical activity and all cause and cause
specific mortality in US adults: prospective cohort study. BMJ 2020; 370: m2031. 2020/07/03. DOI:
10.1136/bmj.m2031. - Sherrington C, Fairhall N, Wallbank G, et al. Exercise for preventing falls in older people living in the
community: an abridged Cochrane systematic Review. Br J Sports Med 2019 2019/12/04. DOI:
10.1136/bjsports-2019-101512. - Peeters G, Dobson AJ, Deeg DJ, et al. A life-course perspective on physical functioning in women.
Bull World Health Organ 2013; 91: 661-670. 2013/10/09. DOI: 10.2471/BLT.13.123075. - Niemela MS, Kangas M, Ahola RJ, et al. Dose-response relation of self-reported and accelerometer-
measured physical activity to perceived health in middle age-the Northern Finland Birth Cohort 1966
Study. BMC Public Health 2019; 19: 21. 2019/01/08. DOI: 10.1186/s12889-018-6359-8. - Michie S, van Stralen MM and West R. The behaviour change wheel: a new method for characterising
and designing behaviour change interventions. Implement Sci 2011; 6: 42. 2011/04/26. DOI:
10.1186/1748-5908-6-42.