An insight into a living systematic review and meta-analysis, as part of the BJSM’s new #KnowledgeTranslation blog series
In our blog, we will explain why and how we did our study, and what makes it different from previous systematic reviews on treatments for Achilles tendinopathy. This large project took more than two years to complete and was funded by the Dutch government as part of the process to create a clinical management guideline. The full-text – which is open access – can be obtained via https://bjsm.bmj.com/content/early/2020/06/15/bjsports-2019-101872
Introduction
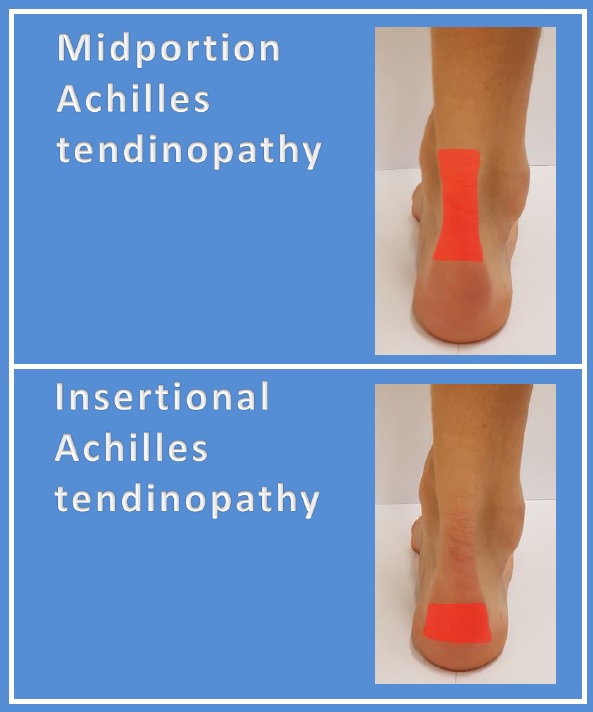
Achilles tendinopathy is very common in both the general population and sports communities, and it severely impacts on daily life and sports participation. Two types of tendinopathy can be differentiated: midportion and insertional Achilles tendinopathy.

There are many ways to treat this condition. As a patient you may wonder “do I need exercise, shockwave, an insole, an injection or maybe surgery for my painful Achilles?” Clinicians trying to answer this question will need to review >100 systematic reviews on separate comparisons, e.g. exercise versus insole. This is a huge challenge, and probably leaves us with the questions “but which of all those treatments investigated is most effective?”
Network meta-analysis can overcome this challenge by testing the comparative effectiveness of all available treatments in one single model. Network meta-analysis (NMA) allows the simultaneous comparison of the effectiveness of all treatments and can rank treatments from most to least effective. See this links for more information on the methods of NMA for clinicians: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5247317/
Methods
So, what did we do in our systematic review and network meta-analysis?
We used a comprehensive conventional and grey literature search, and we also searched trial registers. We appraised the risk of bias using the new ROB 2 tool of the Cochrane Collaboration (https://www.bmj.com/content/366/bmj.l4898). We then used a Bayesian network meta-analysis to compare all available treatments and categorized these treatments (e.g. exercise therapy category). We evaluated treatment effectiveness using the patient-reported VISA-A score of the included studies as primary outcome and return to sport as secondary outcome. We used both treatment and treatment category (also referred to as class) models to compare treatments. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to appraise the quality of evidence.
Results
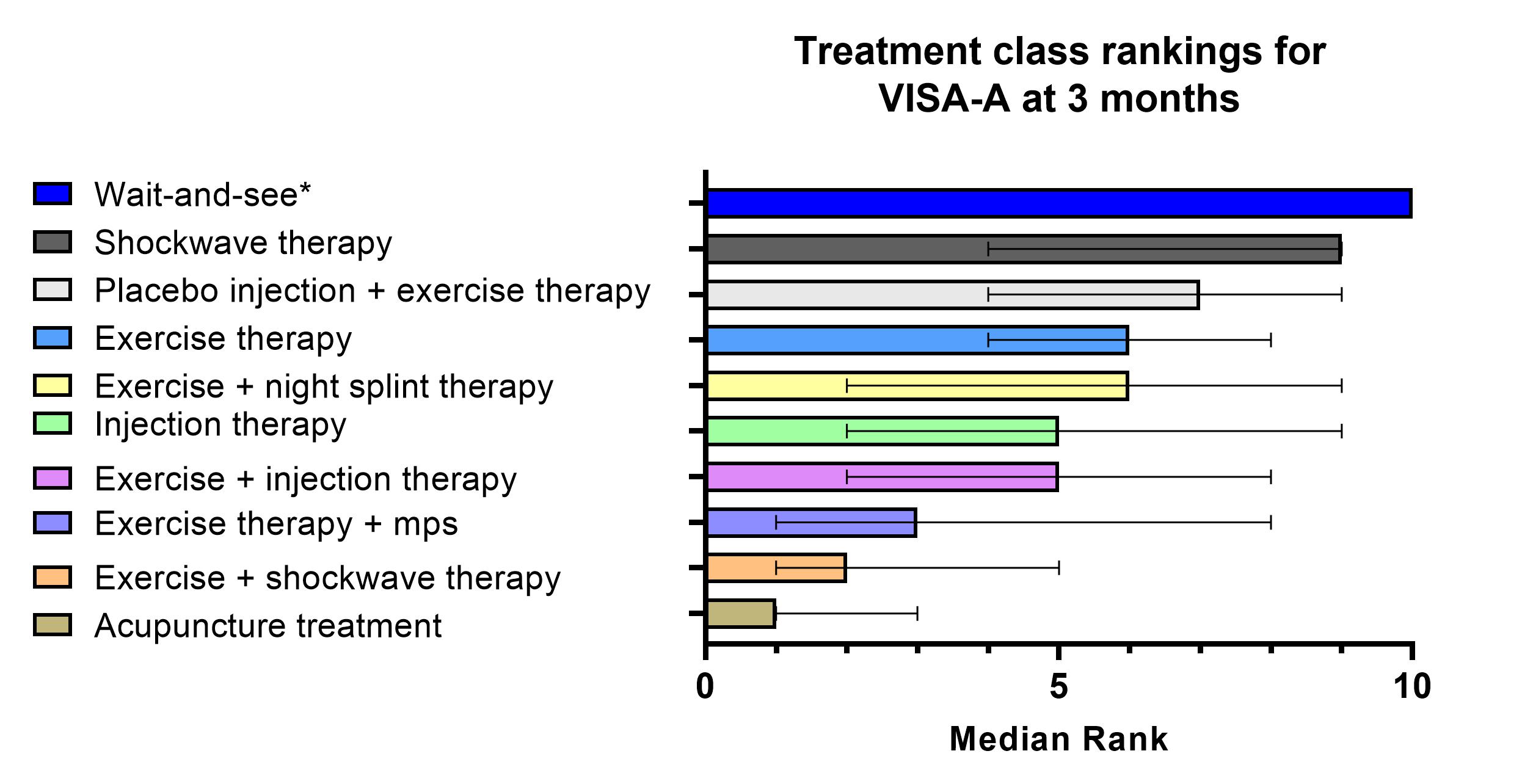
We found 29 trials investigating 42 treatments for patients with Achilles tendinopathy. No trials were at low risk of bias, most had only short follow up and there was large uncertainty in the comparative estimates. Any treatment appears to be superior to wait-and-see for midportion Achilles tendinopathy at 3 months (see figure below).
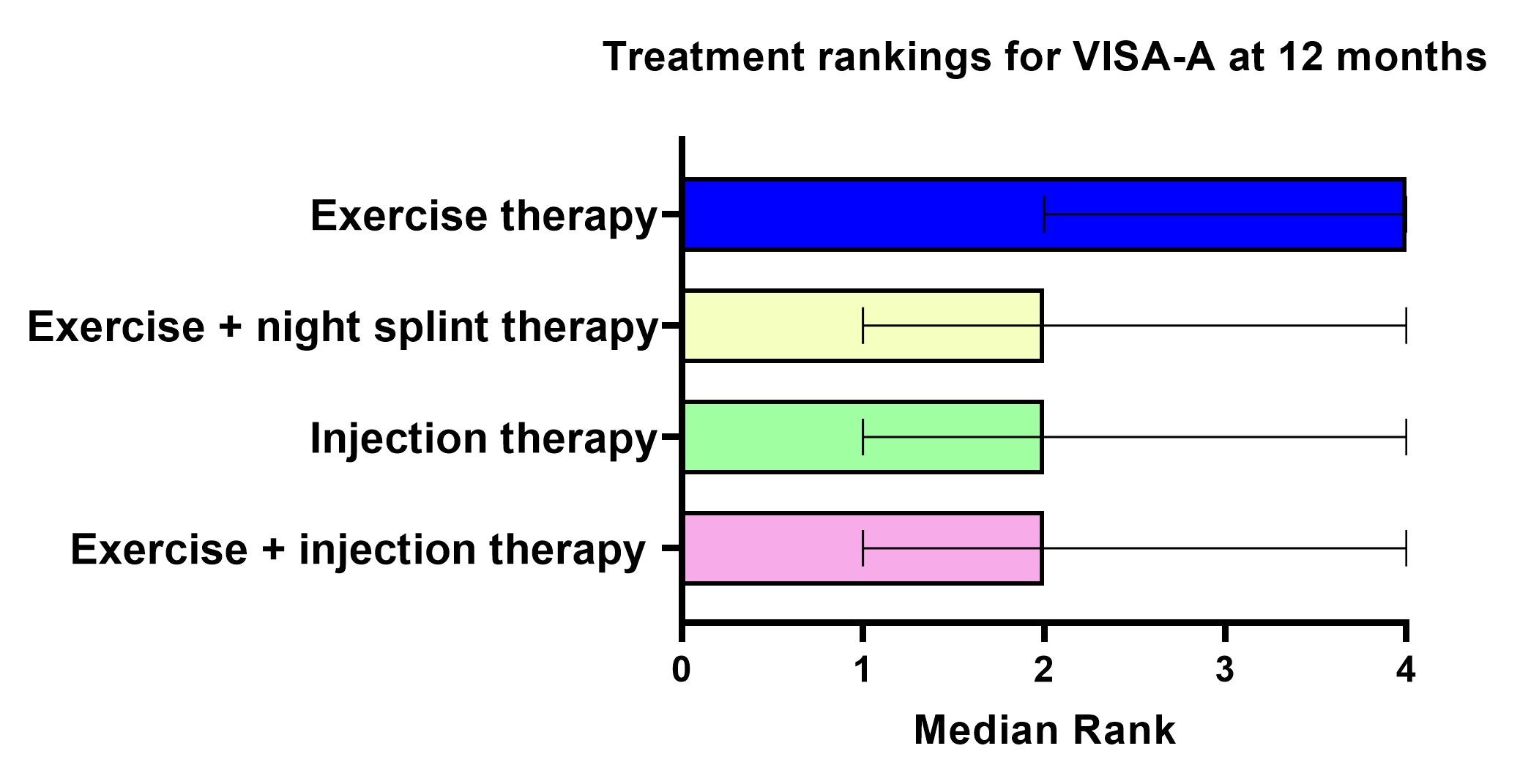
At 12 months, exercise therapy, exercise + injection therapy, exercise +night splint therapy all seems comparable to one another (figure below).
No NMA for insertional Achilles tendinopathy could be performed.
Calf exercises seem the most logical treatment as it’s cheap and has no serious side effects. Therefore, we feel clinicians should consider starting this as initial treatment. Additional treatments do not show superior effect to exercise alone. The type of exercises appears not to really matter, as eccentric exercises and heavy slow load exercises demonstrate similar results.
Recommendations for future research
In future trials, quality of studies in the field of Achilles tendinopathy should be improved. Therefore, we have 8 recommendations for future research:
- Upgrade reporting: follow reporting guidelines, i.e. CONSORT statement http://www.consort-statement.org/
- Study the ROB 2 tool before starting a RCT. Teach yourself how to prevent systematic errors in your research. Involve an epidemiologist in the project. https://www.bmj.com/content/366/bmj.l4898
- Register your study protocol before starting your RCT. An example of such a registry is clinicaltrials.gov
- Do not do an RCT for the sake of doing an RCT – if you start an RCT – make it big. We already have a lot of small studies.
- Adequately describe the study population and specifically how the diagnosis of Achilles tendinopathy was established.
- Trials should use exercise as a standalone comparator to connect with the network
- Include validated outcome measures from the core domains for tendinopathy https://bjsm.bmj.com/content/54/8/444
- Follow outcomes for at least 12 months as Achilles tendinopathy is a longstanding condition
To reduce research resources, avoiding waste of research and efforts, we plan to (1) update the search and review process every 5 years as part of the guideline revision process, and (2) perform annual screening to identify new data that may alter the conclusions and recommendations. These updates will be provided on: https://www.erasmusmc.nl/en/research/projects/treatment-of-achilles-tendinopathy
A huge thanks to the author group (Arco C van der Vlist & Marinus Winters in particular) for submitting this blog as part of the BJSM’s #KnowledgeTranslation series. Please feel free to email steffangriffin@gmail.com if you would like your paper to feature as part of this series