By Garrett Fintan Coughlan @garrett_physio, Andy Friend @andyfriend2011, Brian Green @briangreen36 and Jonathan Hanson @sportsdocskye
In the high pressure environment of professional field sports games, growing numbers of medical personnel are required to provide care. The interprofessional environment has created a higher demand on non-technical skills called ‘human factors’ which include situational awareness, decision making, communication, teamwork and leadership. These skills should be learnt to ensure good clinical outcomes and optimal patient care. Communication strategies commonly exist in disaster relief [1], military and aviation settings [2], however, there is a paucity in the sports medicine literature. Standardised, accurate and unambiguous exchange of information between medical personnel, facilitate informed medical decision making–the highest possible standards of player care and reduced time wasted with non-essential information. In this editorial, we propose a practical medical communication model for field sport games.
PRE-GAME
Pre-game meeting
The pre-game meeting with on and off-field medical personnel (Table 1) from both teams outlines individual and key leadership roles in addition to medical room and pitch protocols (e.g., catastrophic emergency, extrication plan, equipment available, video review). A clearly identifiable leader with clear and concise instructions are two of the most important factors that may differentiate between success and failure of a critical incident [3]. We recommend that all medical personnel agree on the communication protocols outlining the use of verbal (see below In-game) and non-verbal strategies (e.g., hand signals for injurious events / resuscitation team / blood / head injury assessments (HIA)) to manage potentially injurious on-field events. Coaching and medical staff not present at the meeting, should be made aware of any local variations to protocols to ensure clarity pre-game.
Table 1: Sample on-field and off-field medical personnel in professional club rugby
| On-field Home Team | On-field Visiting Team | Off-field Medical Team |
| On-field Team Doctor | On-field Team Doctor | Match Day Doctor |
| On-field Physiotherapist | On-field Physiotherapist | Immediate Care Lead |
| Support Physiotherapist | Support Physiotherapist | Advanced Paramedic |
| Soft-t issue Therapist | Ambulance Team | |
| Video Review Technician | ||
| Medical Room Video Reviewer |
Radio check
Professional teams typically use a secure radio system for in-game communication, allowing for tactical and medical information to be relayed between coaching and medical staff. We recommend that the off-field medical team have an independent radio system to facilitate communication given their potentially different locations in game. Teams should ensure that a pre-game radio check is completed.
IN GAME
Pre-field entry
Identifying and communicating potentially injurious on-field events by players, coaching and medical staff may expedite the initiation of a care plan (e.g. medical staff video review / off-field medical staff activation), and/or coaching staff to prepare a substitution. Informing the refereeing officials of a significant injury may allow for the game to be stopped for appropriate medical care in a safe environment.
Have I got your attention?
With large staff numbers on the radio system, clarity on the source and destination of the message are critical to ensure information is transferred between the relevant personnel. At the start of each message the source should state their name/role and the destination of the message, e.g. ‘Doctor to Coaches….’ , followed by the message with verbal acknowledgement of the receipt of information using the same strategy. Additionally, the use of the aforementioned hand signals may provide immediate feedback to those pitch side regarding on-field events.
The 3 Ps: Player – Problem – Plan
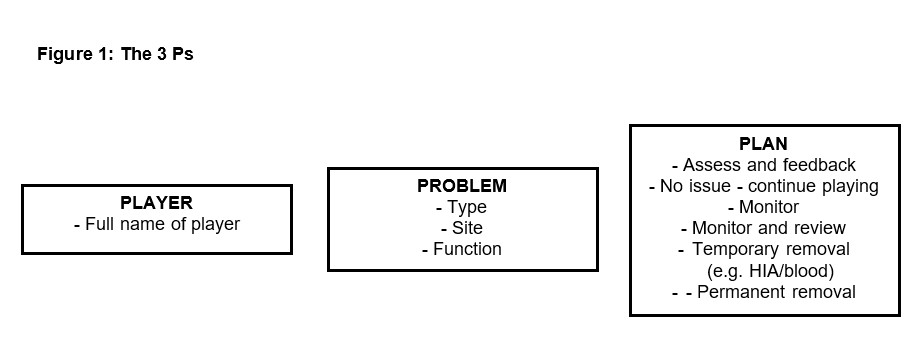
Medical staff should be timely and consistent with their verbal communication. We propose using the ‘3 Ps: Player – Problem – Plan’, when relaying injury information (Figure 1). This strategy can give clarity for those listening and standardises the information flow for each potential injury event, particularly given the differing professions and potentially different medical staff members rotating game cover in-season.
Player: Identifying the player involved by their full name minimizes ambiguity arising from using a player’s nickname or one with the same or similar name.
Problem: Outlining the issue with clinical language relevant to the addressee is essential. For example, a coaching staff message may be the type and site of injury (‘calf muscle strain’), whereas an off-field medical personnel message may require more specific clinical terminology (e.g. ‘appeared ataxic following the collision’).
Plan: A definitive and concise plan should be communicated following each stage of the on-field assessment. For example, following the initial assessment the plan may be that further assessment is required to determine the extent of the injury or that the player may need to be removed immediately.
POST GAME
A post game debrief should be undertaken by medical personnel to review medical events, as well as the efficacy of protocols and the communication process. Finally, the plan of care for injured players should be shared with the medical personnel.
In this editorial, we outlined a potential communication model for medical staff involved with field sport games and conclude that to ensure effective working relationships and optimal player care, the consistency and clarity of information pre, in and post game is essential.
***
Competing interests
None declared
References
1 Shittu E, Parker G, Mock N. Improving communication resilience for effective disaster relief operations. Env Sys Dec 2018;38:379-397. doi.org/10.1007/s10669-018-9694-5
2 Burke CS, Salas E, Wilson-Donnelly K, et al. How to turn a team of experts into an expert medical team: guidance from the aviation and military communities. Qual Saf Health Care 2004;13:96–104. doi.org/10.1136/qshc.2004.009829
3 Jan Ekstrand J, Lundqvist D, Davison M, et al. Communication quality between the medical team and the head coach/manager is associated with injury burden and player availability in elite football clubs. BJSM 2019;53:304-308. doi.org/10.1136/bjsports-2018-099411